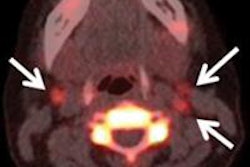
Australian researchers found that FDG-PET scans changed the management plan for more than one-third of patients with Merkel cell carcinoma and altered the disease stage in approximately one in five cases, according to a study in the August issue of the Journal of Nuclear Medicine.
With the information provided by FDG-PET and subsequent changes in treatment plans, overall survival for Merkel cell carcinoma patients was 60% after three years and 51% after five years, according to a team led by Dr. Shankar Siva of the University of Melbourne's department of oncology (JNM, August 2013, Vol. 54:8, pp. 1223-1229).
Merkel cell carcinoma is an aggressive skin disease that often reoccurs and carries a high risk of both nodal and distant metastases. According to the National Cancer Institute, the incidence of Merkel cell carcinoma in the U.S. has increased from 0.15 cases per 100,000 in 1986 to 0.44 cases per 100,000 in 2001.
While the authors describe FDG-PET as a "promising functional imaging modality" to evaluate Merkel cell carcinoma, previous research has been limited to studies with few subjects. One Australian study included 18 patients, 12 of whom received FDG-PET scans for staging. FDG-PET changed the treatment regimen for nine (75%) of the patients.
"Because of the promising nature of these early reports, our group performed a retrospective analysis of our experience to evaluate the role of PET in Merkel cell carcinoma and its ability to stratify prognosis," Siva and colleagues wrote.
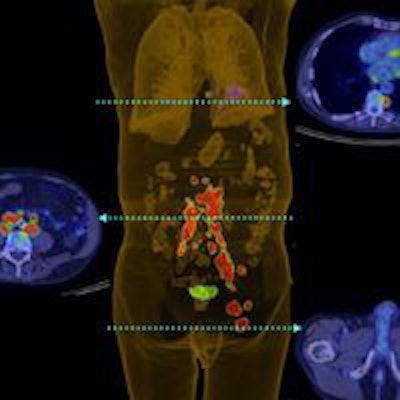
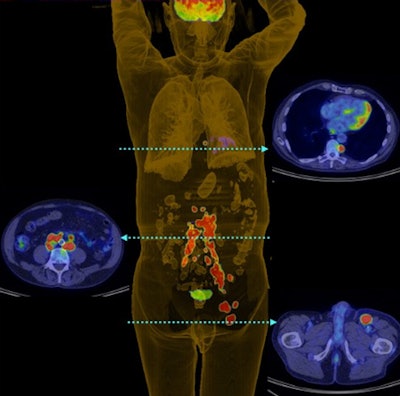 PET 3D reconstruction shows left inguinal nodal and extensive retroperitoneal and thoracic nodal metastases in patient with Merkel cell carcinoma of the left lower limb. Image courtesy of the Journal of Nuclear Medicine.
PET 3D reconstruction shows left inguinal nodal and extensive retroperitoneal and thoracic nodal metastases in patient with Merkel cell carcinoma of the left lower limb. Image courtesy of the Journal of Nuclear Medicine.Patient cohort
Patients with Merkel cell carcinoma were treated at the Peter MacCallum Cancer Centre between January 1997 and October 2010. During those years, they were imaged on either a standalone PET scanner (Quest, GE Healthcare) or on a variety of PET/CT systems (Discovery LS, Discovery STE, Discovery 690, GE; or Biograph 64/40, Siemens Healthcare). PET images were reconstructed using 3D ordered-subset expectation maximization technology.
Of the 102 patients who received staging FDG-PET scans, 21 received standalone PET imaging, while the other 81 were imaged on a hybrid PET/CT system. The median follow-up time was 4.8 years.
The researchers prospectively recorded the patients' treatment plans before and after the FDG-PET scans as part of an institution-wide observational study. Follow-up outcomes were then noted retrospectively.
Siva and colleagues defined a high-impact result as a change in treatment modality, such as going from a surgical option to radiation therapy, or a change in treatment intent, such as switching from curative to palliative. A medium-impact result was defined as no change in modality, but with an alteration of the radiation therapy technique or dose. A low-impact result was defined as no change in modality, technique, or intent.
FDG-PET prowess
FDG-PET scans for tumor staging resulted in a change in treatment for 38 patients (37%), the researchers found. Of the 23 scans that were deemed to have a high impact, 14 (62%) resulted in a change in treatment modality, five (21%) changed treatment intent, and four (17%) changed both treatment modality and radiation therapy technique.
Of the five patients for whom the treatment intent changed, four had their cancer upstaged due to distant metastases and were treated with palliative care. The remaining person was downstaged from suspected but unproven distant metastatic disease and received curative care.
Comparing conventional and PET results showed discrepancies in staging for 22 patients, with PET upstaging 17 patients and downstaging five.
Overall survival for the Merkel cell carcinoma patients was 60% at the three-year mark and 51% at five years, according to Siva and colleagues. In addition, overall survival at three years was 78% for patients with PET-staged I/II disease and 37% for stage III cancer. Overall survival at five years was 67% for stage I/II and 31% for stage III.
Five-year overall survival was 39% for those who received surgery only and 42% for those given radiation therapy or chemoradiotherapy only, they added. The rate was 64% for the combination of surgery and adjuvant radiation therapy or chemoradiotherapy.
The results demonstrate FDG-PET's ability to "stratify prognosis with stage, as FDG-PET was the strongest prognostic factor for survival," the authors concluded. "If these results can be validated by similarly large series from other institutions, staging FDG-PET should become part of the standard management of Merkel cell carcinoma."