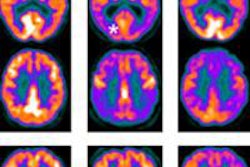
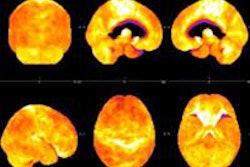
PET scans show that elderly people with hardening of the arteries are more likely to have beta-amyloid plaque in the brain, even if they show no signs of dementia or Alzheimer's disease, according to a study published online October 16 in Neurology.
Researchers found that arterial stiffness was greatest among people with both increased beta-amyloid deposits and white-matter hyperintensities or lesions in the brain, both of which contribute to the development of dementia.
The findings provide more insight into the associations between arterial stiffness and beta-amyloid deposits and add to previous research suggesting a link between arterial stiffness and cerebrovascular disease, wrote lead author Timothy Hughes, PhD, a postdoctoral fellow at the University of Pittsburgh's Institute for Clinical Research Education, and colleagues (Neurology, October 16, 2013).
Arterial stiffness
Previous studies have linked hypertension with cognitive impairment and features of Alzheimer's disease, as well as small-vessel disease and white-matter hyperintensities, Hughes and colleagues noted. Arterial stiffness appears to play a role in hypertension and the adverse effects it can have on the brain, including impaired cognitive function and dementia in older adults.
However, the "relationship between arterial stiffness and [beta-amyloid] deposition is unknown," the authors wrote. Therefore, their study sought to evaluate the relationship between arterial stiffness and measures of brain structure, including beta-amyloid deposition and white-matter hyperintensity volume, in elderly adults with no dementia.
Hughes and colleagues recruited 91 participants (60 men and 31 women) between the ages of 83 and 96 years. Of this group, 15 had the e4 version of the apolipoprotein E (APOE) gene, which is associated with Alzheimer's disease, and 14 were diagnosed with mild cognitive impairment at the time of neuroimaging.
In 2009, the participants received 1.5-tesla brain MRI scans (Signa, GE Healthcare) and PET imaging with Pittsburgh Compound B (PiB), which is used as a marker of amyloid plaque in the brain. Before PiB-PET imaging, subjects underwent a cognitive evaluation, a timed walk, and a rundown of their prescription and over-the-counter medications.
In 2011, the researchers measured the individuals' blood pressure at rest, mean arterial pressure, and arterial stiffness in the central (carotid-femoral and heart-femoral), peripheral (femoral-ankle), and mixed (brachial-ankle) vascular beds using a noninvasive pulse-wave velocity analyzer.
Beta-amyloid detection
PiB-PET scans revealed that 44 participants (48%) were positive for beta amyloid. Those individuals with beta-amyloid plaques were more likely to have high systolic blood pressure, higher mean arterial pressure, and greater arterial stiffness as measured by the brachial-ankle method. For every standard deviation increase in brachial-ankle arterial stiffness, subjects were twice as likely to have beta-amyloid plaques in the brain.
"Arterial stiffness was highest in individuals with both high [beta-amyloid] deposition and [white-matter hyperintensities], which has been suggested to be a 'double hit' contributing to the development of symptomatic dementia," Hughes and colleagues wrote.
When compared with subjects without beta-amyloid plaque and with low white-matter hyperintensities, each standard deviation increase in arterial stiffness was associated with a two- to fourfold increase in the likelihood of having amyloid plaque and a high number of brain lesions.
Hughes and colleagues noted that the relationship between arterial stiffness and beta-amyloid plaque did not change when regular resting blood pressure was considered. The APOE e4 variation also did not affect the relationship between arterial stiffness and beta-amyloid plaque.
"The associations between arterial stiffness and brain structural abnormalities were largely independent of blood pressure and appeared to differ by type of brain abnormality and vascular bed measured," the authors concluded. "[Beta-amyloid] deposition in the brain (a hallmark of Alzheimer's disease) was more strongly associated with mixed measures of arterial stiffness ... than central measures, while white-matter disease burden was more strongly associated with central measures of arterial stiffness alone."
Additional research should be conducted to determine whether the connections between arterial stiffness and white-matter hyperintensities are separate from the links between arterial stiffness and amyloid deposition in the brain, according to the authors.
Study disclosures
Two study co-authors are co-inventors of PiB and therefore have a financial interest in its license agreement.