Combining coronary CT angiography (CCTA) and stress CT myocardial perfusion imaging (MPI) improves the evaluation of coronary artery stenosis in high-risk patients, reducing the number of false positives and potentially the number of unnecessary interventions, according to new research from the Medical University of South Carolina (MUSC) in Charleston.
In patients at high risk for coronary artery disease who underwent CCTA and stress CT MPI, along with SPECT and (usually) invasive coronary angiography, the combined diagnostic approach of CCTA plus CT MPI boosted sensitivity for detecting significant stenosis to 100%, versus 91% to 95% for either CT exam alone. Also importantly, specificity rose by 17% when the two exams, acquired on a dual-energy CT (DECT) scanner, were used together, potentially preventing interventions that would not help the patient, according to the researchers.
 Dr. Carlo de Cecco from the Medical University of South Carolina.
Dr. Carlo de Cecco from the Medical University of South Carolina.
"A growing body of evidence supports the use of DECT perfusion with first-pass technique in the evaluation of myocardial ischemia via inducible myocardial perfusion defects," said Dr. Carlo de Cecco in a presentation at the 2014 European Congress of Radiology (ECR). "By performing this protocol with CCTA, we can combine the two approaches to obtain morphological and functional information about the heart."
However, "our evaluation of the high-risk patients is limited by the presence of diffuse and severe calcifications that can lead to severe artifacts and cause false-positive findings," he noted. "For this reason, the guidelines consider CCTA inappropriate in this class of patients."
Enter stress myocardial perfusion imaging with CT, which could potentially overcome the diagnostic limitations of first-pass perfusion and CCTA to improve diagnostic accuracy in high-risk patients to determine noninvasively if stenosis visualized on CT are flow-limiting, de Cecco said. The study aimed to determine the incremental value of adding adenosine stress CT MPI to CCTA for assessing high-risk populations using SPECT and CTA.
De Cecco, along with Dr. U. Joseph Schoepf and their MUSC colleagues, prospectively examined a total of 29 consecutive patients who were referred for cardiac SPECT examinations for known or suspected coronary artery disease to additionally undergo pharmacological stress cardiac DECT. In 25 patients (mean age 60 ± 11 years), cardiac catheterization was available as the reference standard for morphologically significant stenosis.
The cohort was quite high-risk, de Cecco said. One-third smoked, one-third had diabetes, 41% had dyslipidemia, 86% had hypertension, 86% had a family history of coronary artery disease, and 55% had a personal history of myocardial infarction.
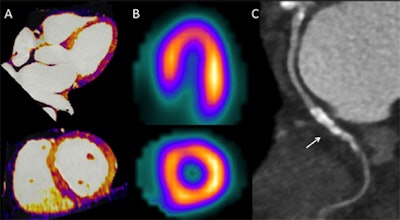 A 62-year-old man with a history of coronary revascularization and recent onset of chest discomfort. Pharmacological stress dual-energy myocardial iodine distribution maps (A) demonstrate homogenous iodine distribution consistent with normal myocardial perfusion. Stress SPECT images (B) also demonstrate normal myocardial perfusion. Coronary CTA (C) demonstrates patent stents (arrow) in the circumflex branch. All images courtesy of Dr. Carlo De Cecco.
A 62-year-old man with a history of coronary revascularization and recent onset of chest discomfort. Pharmacological stress dual-energy myocardial iodine distribution maps (A) demonstrate homogenous iodine distribution consistent with normal myocardial perfusion. Stress SPECT images (B) also demonstrate normal myocardial perfusion. Coronary CTA (C) demonstrates patent stents (arrow) in the circumflex branch. All images courtesy of Dr. Carlo De Cecco.The CT protocol was classic rest and stress: First came calcium scoring, followed by adenosine stress acquisition, CCTA five minutes later, and then late-enhancement and myocardial viability imaging six minutes later, he said. The images were reconstructed in a merged fashion and analyzed by two experienced readers working in consensus. The researchers calculated the performance metrics of CCTA and stress CT MPI alone and in combination, looking in each case at sensitivity, specificity, and area under the curve (AUC) values.
The results showed the following:
- Myocardial perfusion defects were identified by SPECT in 21 of the 29 (72%) patients, including 14 reversible, 16 fixed, and 3 as mixed defects.
- Among the 25 of the 29 patients who underwent cardiac catheterization, 19 were found to have at least one significant (≥ 50%) diameter luminal narrowing.
- CCTA demonstrated at least one significant stenosis in 23 of the 29 patients.
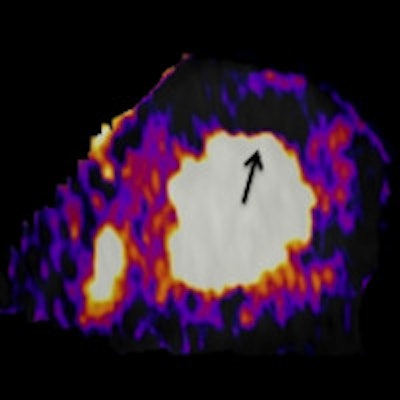
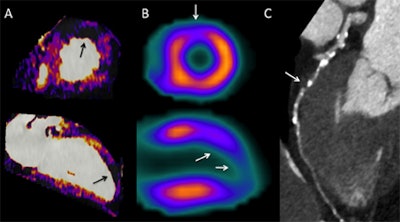 A 68-year-old man with diabetes experiencing shortness of breath after mild exercise. Pharmacological stress dual-energy CT myocardial iodine distribution maps (A) demonstrate a circumscribed area of decreased iodine content in the apicoanterior left ventricular myocardium consistent with a perfusion defect (black arrows). Stress SPECT images (B) confirm an area of ischemia (white arrows). Coronary CT angiography (C) demonstrates critical stenosis of the proximal portion of the left anterior descending artery (arrows).
A 68-year-old man with diabetes experiencing shortness of breath after mild exercise. Pharmacological stress dual-energy CT myocardial iodine distribution maps (A) demonstrate a circumscribed area of decreased iodine content in the apicoanterior left ventricular myocardium consistent with a perfusion defect (black arrows). Stress SPECT images (B) confirm an area of ischemia (white arrows). Coronary CT angiography (C) demonstrates critical stenosis of the proximal portion of the left anterior descending artery (arrows).Greater specificity for combined tests
| Per-patient performance of CCTA and stress myocardial perfusion CT, together and separately | ||||
| Protocol | Sensitivity | Specificity | AUC | p-value |
| CCTA positive (at least 1 stenosis ≥ 50%) |
95% | 50% | 0.72 | 0.11 |
| Perfusion defect at DECT | 95% | 50% | 0.72 | 0.11 |
| Either positive | 100% | 33% | 0.67 | 0.23 |
| Both positive | 90% | 67% | 078 | 0.04 |
"We found that the combined approach ... both perfusion and CCTA, had a higher specificity compared to only CCTA or perfusion-only assessment," de Cecco said. The combined tests yielded 17% higher specificity than that of either test separately, and a significant p-value of 0.04 using both exams.
Study limitations included the small cohort and the lack of inter- and intrareader variability assessment, which are important for reproducibility, he said. In addition, catheter angiography was not performed in four patients.
"The combined analysis of CCTA and DECT myocardial perfusion reduces the number of false positives in a population at high risk for coronary artery disease, and outperforms the anatomical test of CCTA alone for detection of morphologically and hemodynamically significant coronary artery stenosis," de Cecco said.




















