By extracting statistical information and other measurements from PET images using a data analysis technique called radiomics, researchers have developed a way to determine radiation therapy dose more accurately, according to a study presented this week at the American Association of Physicists in Medicine (AAPM) meeting in Austin, TX.
In the study of patients with non-small cell lung and head and neck cancer, senior author Joseph Deasy, PhD, chair of the department of medical physics at Memorial Sloan Kettering Cancer Center, and colleagues showed how radiomics could help predict the likely progression of cancer, or its response to treatment.
Deasy said the findings represent another advance in how radiomics, a big-data technique for extracting quantitative data from medical imaging scans, could incorporate details from PET images to guide treatment decisions.
"This is different from what has been done in the past," he said. "Diagnostic imaging typically was only used to identify the presence of cancer or to outline the extent of the disease and determine where to target radiation dose. What we have done, using emerging methods in this new area of research called radiomics, is to extract various subtle mathematical characteristics of the tumor appearance."
Shape and texture
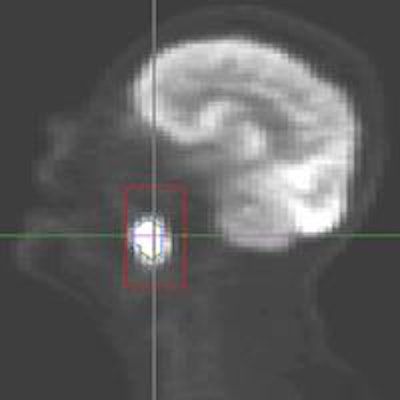
Tumor shape and texture are two key characteristics in the use of radiomics. Observers look to see if the tumor is round or concave and if it reaches out to nearby tissue, Deasy explained. In analyzing texture, they note if the tumor is flat, uniform, and bright, or if it is rough with areas of low or high FDG intensity.
In the largest study to date using radiomics tools, the researchers collected PET scan results between August 2006 and August 2012 on 163 patients with 172 biopsy-proven T1 or T2 non-small cell lung cancers before they were treated with stereotactic body radiotherapy at the center.
Deasy and colleagues also retrieved pretreatment and post-treatment PET scans between December 2002 and March 2009 on 174 patients with stage III-IV head and neck cancer who were treated with chemoradiation therapy. PET scans were converted to a Computational Environment for Radiotherapy Research (CERR) format, and they used CERR software to analyze 24 features covering shape, texture, and histogram in FDG-avid disease regions.
Using the data from PET scans acquired before and after treatment, along with information on how the patients fared, including whether tumors receded or how long the patients survived, the researchers were able to create models to determine the most appropriate cancer therapy.
"The variability of the PET image intensity across the tumor implies greater risk of the spread of the disease," Deasy said. "[This] can then be used to make decisions about systemic therapy."
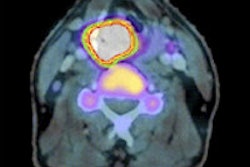
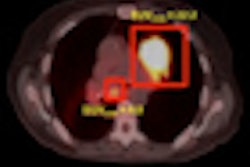
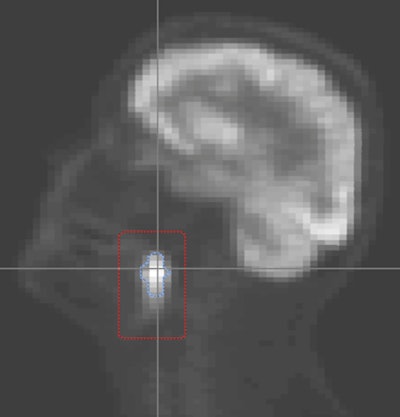 Radiomics evaluates the tumor's size (above) and texture (below). More intense PET images imply the need for more radiation to control the cancer. Images courtesy of Joseph Deasy, PhD, and AAPM.
Radiomics evaluates the tumor's size (above) and texture (below). More intense PET images imply the need for more radiation to control the cancer. Images courtesy of Joseph Deasy, PhD, and AAPM.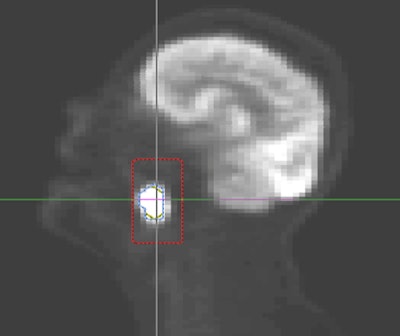
Statistical modeling
By using statistical modeling based on the extracted mathematical properties, researchers can predict how much radiation dose is required for a particular tumor, especially in head and neck and non-small cell lung cancer, Deasy said.
"This can help us from overtreating cancers and potentially causing toxicity in normal tissue, and help us not to undertreat cancers that may need a fairly high dose of radiation to have a high probability of disease control," he added.
Given the promising results of the study, Deasy believes radiomics could also be useful for other types of cancer.
"We think detailed image analysis related to predicting response to therapy or prognosis has a lot of applications to other cancer sites," he said.
In addition, the technique could be applied to other imaging modalities.
"We and groups at other leading institutions are spending a lot of effort looking at not just PET images, but also CT, volumetric x-ray, and MRI," he said.
Even though each modality offers different information about tumors, the basic methodology of radiomics would remain constant.
"There is always some modification [when] going to a different form of imaging, but basically the idea is still the same," Deasy said. "Extract texture features, shape features, and anything about the image that we think might be important and put it into a predictive modeling framework."
The next big step for Deasy and colleagues is to confirm radiomics' worth in the clinical setting.
"We are already discussing with our radiation oncology physicians how we might choose the dose distribution levels and radiotherapy based on these PET images," he said. A final decision on how to do that is pending.