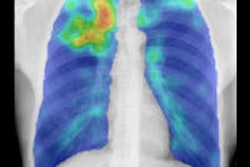
A new study in the September 24 issue of the Journal of the American Medical Association found that FDG-PET has sharply lower specificity for diagnosing lung cancer in geographic regions where infectious lung disease is common. The findings could affect how PET is used for following up CT lung screening studies.
The review of 70 studies found that in regions where infectious lung disease is highly prevalent, FDG-PET's specificity was only 61% for differentiating which nodules were suspicious for lung cancer. This compares to a specificity of 78% to 86% in the literature.
Given the low specificity and other factors, FDG-PET should not be used to diagnose lung cancer in these areas unless an imaging facility can achieve accuracy comparable to what is seen in nonendemic areas, the researchers concluded (JAMA, September 24, 2014, Vol. 312:12, pp. 1227-1236).
"FDG-PET for the diagnosis of lung cancer in patients who reside in a region with significant endemic infectious lung disease should be recognized as having lower specificity (approximately 61%) than previously reported," wrote lead author Stephen Deppen, PhD, from the Tennessee Valley Healthcare System and Vanderbilt University Medical Center, and colleagues.
Previous studies
In previous research, FDG-PET has achieved sensitivity and accuracy of around 90% to 96% in identifying malignant or benign lung nodules, while specificity has ranged between 78% and 86%. However, other recent studies have shown mixed results regarding FDG-PET's accuracy in diagnosing lung cancer in patients who reside in regions of the U.S. and Canada where fungal and other infectious lung diseases are endemic, the authors noted.
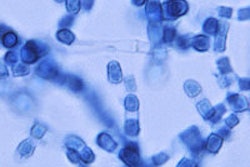
For example, histoplasmosis and blastomycosis, diseases caused by inhaling airborne fungal spores, are endemic across much of the Mississippi, Ohio, and Missouri River Valley regions and throughout southern Ontario in Canada. The infections can result in granulomas, or areas of inflammation, in the lungs. The researchers also cited studies from South Africa and Japan in which endemic tuberculosis reduced FDG-PET/CT's specificity to 25% and 21%, respectively.
To obtain more information on FDG-PET's usefulness in such regions, Deppen and colleagues reviewed databases from Medline, Embase, and the Web of Science for papers published between October 2000 and April 2014. In all, 70 studies met the inclusion criteria, encompassing a total of 8,511 nodules, 5,105 (60%) of which were malignant.
Among those studies were 10 papers that focused on the use of FDG-PET in areas where infectious lung diseases were endemic; these included 1,431 individuals, of whom 1,082 (76%) had cancer.
FDG-PET's shortcoming
Their analysis found pooled sensitivity (across all 70 studies) of 89% and pooled specificity of 75% for FDG-PET in diagnosing lung cancer. When comparing geographic regions with and without endemic infectious lung disease, however, the researchers found major variations in specificity: Regions with endemic lung disease had a specificity of 61%, compared with specificity of 77% in regions where it wasn't prevalent.
As one might expect, the size of the lesion had a slight effect on FDG-PET's efficacy. In the meta-analysis, 34 studies reported an average or median lesion diameter of 2 cm or smaller. In these papers, the average adjusted sensitivity was 87%, ranging from 84% to 90%. In 23 studies with average or median diameters greater than 2 cm, average adjusted sensitivity was slightly better at 91% (range, 89%-93%).
Specificity was 74% in studies with lesions 2 cm or smaller and 75% in studies with larger lesions.
Deppen and colleagues emphasize that imaging facilities should be aware of FDG-PET's poorer performance in regions where there are significant endemic infectious lung conditions. The finding is particularly important as CT lung cancer screening becomes more commonplace.
"Knowledge of this reduction in specificity should limit the use of FDG-PET to diagnose lung cancer unless substantial institutional expertise in FDG-PET interpretation has been proven," the authors wrote. "Should low-dose CT screening for lung cancer become the diagnostic standard, knowledge of FDG-PET/CT performance is even more critical because the vast majority of indeterminate lung nodules detected through screening are benign."