PET/MRI is making progress in moving from being a research technology to a modality that's used clinically. Radiologists who use it frequently are recognizing its value for several applications, but work remains in convincing referring physicians of its worth.
At the University of California, San Francisco (UCSF), approximately five clinical PET/MR studies have been performed each week, according to Dr. Spencer Behr from the university's radiology department. Behr described the group's experiences with PET/MRI as part of an overview of the technology at the recent American Association of Physicists in Medicine (AAPM) meeting in Anaheim, CA.
At UCSF, PET/MR research on humans has been going on for about a year and a half, while clinical PET/MRI exams began in April and are reimbursed within the hybrid imaging category, Behr said. The challenge is to make the clinicians understand the benefits of the added information for more confidence in diagnosis.
"Clinical applications of PET/MR are slowly gaining steam," he explained.
Conditions for which PET/MR is suitable include colorectal, liver, and cervical cancers. Patients come in for a one-stop local and systemic staging exam, and radiation exposure is lower than with PET/CT, Behr explained. Besides tumor staging, the technology supports surgical planning and the switch from surgery to chemotherapy or radiation therapy. Epilepsy staging is another suitable application.
PET/MR has also made progress in the clinical routine at Washington University School of Medicine in St. Louis, said Richard Laforest, PhD. At his site, most PET/MRI acquisitions are still research cases, with clinical cases numbering around four or five per week. Many of these are pelvic cancer patients, with an increasing number of pediatric cases to take advantage of the modality's lower radiation dose.
There are some challenges with PET/MRI, according to Laforest, in particular regarding attenuation correction of bones. Zero echo time or ultrashort echo time MRI sequences are recent developments targeting this problem. Issues such as these -- soon to be solved by PET/MRI manufacturers -- are among factors that could hinder expansion of the technology.
In general, the integrated PET/MRI systems available in the market function well, despite the complexity of the technology. Time of flight (TOF) acquisition protocols for PET significantly help overcome some of the challenges of the technology. TOF helps improve image quality and makes the system more robust with regard to defects in the attenuation map.
"A lot of areas need exploring to make the technology perfect -- in attenuation correction and in motion correction," according to Floris Jansen, PhD, chief engineer of PET/MR at GE Healthcare. "And workflows need to be optimized for patient throughput in order for the equipment to pay for itself."
Another clinical issue is metal implants, which can present challenges in the magnetic field of an MRI scanner.
"We are currently working on a technique for research called 'joint estimation' that leverages the TOF capabilities of the PET detector and whatever MR information we can get to estimate both the attenuation and the emission of the body at the same time," Jansen said.
This works around the issue of metal in MR images by using PET-intrinsic data to estimate attenuation, creating a full 3D attenuation map and actually visualizing the metal.
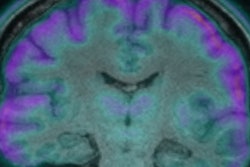
The potential of PET/MRI is enormous, Jansen continued. At the International Society for Magnetic Resonance in Medicine (ISMRM) conference, Gary Glover, PhD, from Stanford University showed a simultaneous view of dopamine receptor activity in the brain using both functional MRI (fMRI) and PET. This can provide new insights into the biochemistry of the brain, Glover said, and promises to advance research on depression.
In general, the brain is one of the key organs for which MRI is useful "thanks to soft-tissue contrast, combined with the quantitation and the sensitivity to physiological processes which you get from PET," Jansen said.
Glover's activities require these processes to be fully simultaneous, while in other situations, it may be sufficient to have good spatial registration and to do sequential scans, Jansen continued.
"For longer-lived tracers such as F-18, you may have longer uptake times and PET acquisition may show physiological events which happened, say, 30 minutes ago," Jansen said. "On the other hand, organs such as the prostate move continuously, and spatial registration is lost if images are taken sequentially. Bowel and pelvis imaging, in particular, therefore requires simultaneous acquisition."
But as with all good things, the clinical development of PET/MRI will take time.
"With every new imaging modality, literature has to be created, data has to be vetted, and the utilization has to be determined," Behr said.
The process for PET/MR is similar to what occurred for PET/CT when that hybrid modality was introduced.
"People today forget how long it took for PET/CT, by way of research and trials, to become an oncology heavyweight," he concluded.