In a word, "disappointment" is how members of the nuclear medicine and radiology communities are reacting to last month's rejection by the U.S. Centers for Medicare and Medicaid Services (CMS) of a proposal to loosen restrictions on reimbursement for sodium fluoride (NaF) PET scans to detect bone metastases.
On September 16, CMS issued a proposed decision memo that declined to pay for the use of NaF-PET scans to identify bone metastases. However, the agency proposed to continue its coverage with evidence development (CED) policy for another 12 months.
Disappointment "would be an understatement," said Dr. Barry Siegel, chief of the division of nuclear medicine at the Mallinckrodt Institute of Radiology at Washington University. "We thought we were on the right track in terms of demonstrating what needed to be demonstrated."
 Dr. Barry Siegel from the Mallinckrodt Institute of Radiology.
Dr. Barry Siegel from the Mallinckrodt Institute of Radiology.Siegel also serves as co-chair of the National Oncologic PET Registry (NOPR), which has been collecting data from imaging facilities for almost five years on how NaF-PET has influenced patient management.
"It is clear from the decision and from a subsequent conversation with the staff at CMS that they were looking for more definitive evidence of change in patient management, and, if possible, frank documentation of improved patient outcomes, which is always problematic in a single-arm, open-label registry, because there is no control group," he said.
Exploring their options
Siegel and other NaF-PET proponents are now exploring their options, which could involve reviewing claims data from the NOPR cohort to validate how the actual care a patient received matches or changes what the referring physician initially planned for that patient. In other words, did the information provided by the NaF-PET scan simply change the physician's thoughts about how to proceed, or did the modality actually alter the patient's treatment plan?
"We have expressed to CMS our understanding about what we might be able to do with the data that is currently available to us, or could become available to us," Siegel said. "We will see how it plays out over the next few months as the final decision comes forward."
Last year, a NOPR study found that NaF-PET changed treatment in more than half of male patients with prostate cancer. Use of the technique shifted management plans for 77% of initial staging patients, 52% of men with suspected first osseous metastases, and 71% of those with suspected progression of osseous metastases.
"After NaF-PET, referring physicians also reported that 70% to 80% of patients would avoid additional noninvasive imaging and that plans to gather additional information (biopsy or more imaging) would be necessary in only 7% to 12%," the authors wrote in the Journal of Nuclear Medicine (February 27, 2014).
 Dr. Hossein Jadvar, PhD, of the University of Southern California.
Dr. Hossein Jadvar, PhD, of the University of Southern California."I am not sure why there is even a question about the diagnostic performance of NaF-PET/CT," said Dr. Hossein Jadvar, PhD, an associate professor of radiology at the University of Southern California (USC) Keck School of Medicine.
In fact, oncologists at USC's Norris Comprehensive Cancer Center have switched from planar bone scintigraphy using technetium-99m and separate CT scans to NaF-PET imaging.
"In a matter of one to one-and-half hours, they have all the information they need," said Jadvar, who currently serves as president of the Society of Nuclear Medicine and Molecular Imaging (SNMMI). "There is no question that NaF-PET is more sensitive and more specific than a conventional bone scan. All the findings on PET can be localized to determine if results are normal or abnormal."
Jadvar has published several papers on NaF-PET, including a 2012 study in which the imaging technique was more effective than FDG-PET for detecting occult metastatic disease in men with prostate cancer and relapse (Clinical Nuclear Medicine, July 2012, Vol. 37:7, pp. 637-643). He is now investigating the utility of NaF-PET/CT for detecting early, small bone metastases in patients with prostate cancer who have a very slight elevation in prostate-specific antigen (PSA) levels after radical prostatectomy.
Typically, oncologists do not perform a bone scan until PSA levels are greater than 20 ng/mL, due to the likelihood of false-negative results, he said.
"But because of the superiority of NaF-PET/CT, we can detect very early metastases to the bone in these patients with prostate cancer at much lower PSA levels," Jadvar said. "We are continuing this project to see what is the threshold of PSA we can get down to."
The findings could be very beneficial for patient management "because then patients would know if they need to begin systemic therapy earlier," he added. "That hopefully will make a difference in their outcome."
No surprises
Dr. Gary Dillehay, professor of radiology at Northwestern Memorial Hospital and former SNMMI president, told AuntMinnie.com that the CMS decision was "disappointing but not unexpected."
 Dr. Gary Dillehay from Northwestern Memorial Hospital.
Dr. Gary Dillehay from Northwestern Memorial Hospital.He likened the situation to CMS' decision in July 2013 that failed to fully endorse PET beta-amyloid imaging for dementia or neurodegenerative disease. The agency ruled there was "insufficient" evidence to conclude that PET beta-amyloid imaging improved health outcomes for patients with dementia or neurodegenerative disease. However, CMS did agree to cover one PET beta-amyloid scan per patient under certain circumstances.
"They [CMS] do not disagree that you can image what you say you can image, but it must have a measurable improvement in patient outcomes that we have not been able to demonstrate yet," Dillehay said.
And if reimbursement is in question, hospitals and patients are considerably less likely to pay for NaF-PET scans.
"I doubt private insurers will pay either, since they frequently follow what CMS does, and particularly if CMS comes down this hard and says [NaF-PET] is not approved," he added.
'Spectacular' images
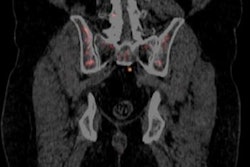
Siegel readily endorsed the quality of NaF-PET images as "spectacular," but he added that the results are "a lot of work to read, because they show so much. On the other hand, because they show so much is why they are so valuable."
In some cases, the choice of whether to order an NaF-PET scan may be one of convenience.
"People have been used to the conventional bone scan for a long time, and changing habits is hard," Siegel said. "If I order a sodium-fluoride PET scan, I have to deal with the NOPR paperwork, if I am a referring physician."
NOPR did successfully campaign for FDG-PET coverage from CMS through evidence-based data on patient management and subsequent concordance with outcomes. Now NaF-PET advocates are hoping for the same result.
"The real question is whether that will be sufficient to satisfy CMS for NaF-PET, and that remains unknown," Siegel said.