While the use of PET/MRI is feasible across all types of cancer, it may be tough to show its superiority to PET/CT due to the latter modality's proven track record in detecting and evaluating the disease, according to a review in the March issue of the Journal of Nuclear Medicine.
Researchers from the University of California, Los Angeles (UCLA) surveyed the use of PET/MRI across a broad range of cancers using published literature. They found that while PET/MRI is comparable to PET/CT in many cases, it's particularly beneficial for prostate cancer and bone metastases; however, it falls short in lung nodule assessment.
To what degree PET/MRI becomes a mainstay in oncologic imaging will also greatly depend on economics and if "reasonable workflows can be established," wrote lead author Dr. Claudio Spick and colleagues from UCLA's David Geffen School of Medicine. Future studies also should explore the multiparametric potential of MRI. (JNM, March 2016, Vol. 57:3, pp. 420-430).
PET/CT's ascension
After PET/CT was introduced some 15 years ago, it quickly became clear that the hybrid modality improved the diagnosis and assessment of cancer, Spick recalled. While PET/MRI can provide similar evaluations, its adoption has been slower than PET/CT for various reasons.
 Dr. Claudio Spick from UCLA.
Dr. Claudio Spick from UCLA."One reason is because PET/CT already assesses cancer patients with very high accuracy," Spick told AuntMinnie.com. "So it is difficult to be better than PET/CT already is."
In addition, PET/MRI's higher price tag, operating costs, and logistics are a hindrance for many imaging centers and institutions. Spick said that is why the scanners are found primarily in research centers or universities with greater financial resources.
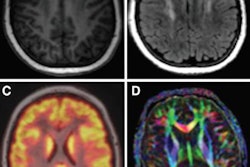
Yet PET/MRI's advantages include high soft-tissue contrast and the ability to perform functional MRI, according to the authors.
"However, rather than focusing on potential synergy between the capabilities of functional MRI and molecular PET, most research has used MRI almost exclusively to provide the anatomic framework for the PET signal," they wrote. "Thus, most studies have compared the diagnostic accuracy of predominantly anatomic PET/MRI with that of FDG-PET/CT in cancer."
For their review, Spick and colleagues examined PET/MRI versus PET/CT in a wide range of cancer studies, including head and neck, gastrointestinal, gynecologic, and breast cancers, as well as lymphoma and neuroendocrine tumors. The most noteworthy findings were for prostate, bone, and lung cancers.
Prostate cancer
Because FDG-PET is not commonly used in the workup of patients with prostate cancer, most published papers explored the use of different PET probes in conjunction with PET/MRI, the researchers found.
Spick and colleagues identified three studies with a total of 88 patients in which the performance of carbon-11-labeled (C-11) or F-18-labeled choline and gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA) PET/CT was compared with that of PET/MRI.
According to National Comprehensive Cancer Network (NCCN) guidelines, multiparametric MRI is effective for staging, characterizing, and evaluating the suspected recurrence of prostate cancer, while CT is preferred for clinical assessment after the diagnosis of prostate cancer, when there is insufficient information to assess the prostate gland.
After their review, the UCLA researchers concluded that C-11- or F-18-labeled choline and Ga-68 PSMA PET/MRI studies for prostate cancer are feasible. Anatomic lesion detection within the prostate was more accurate with PET/MRI -- an advantage that could help in biopsy planning.
On the downside, PET/MRI T1- and T2-weighted sequences were "not superior to PET/CT for prostate characterization and bone lesion localization," they noted.
Metastatic bone cancer
Skeletal scintigraphy with subsequent radiography, if needed, is recommended for staging patients at high risk for bone metastasis. Individually, CT and MRI can help when initial findings are inconclusive.
FDG-PET/CT is considered complementary to bone scintigraphy, while MRI may be "more sensitive for detecting early lesions and marrow-based metastases than plain radiography, CT, or radionuclide bone scanning," the authors wrote.
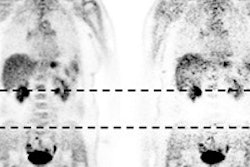
While data are somewhat limited in this area, Spick and colleagues found three studies that compared FDG-PET/CT with PET/MRI among a total of 295 patients with suspected bone metastases.
One paper reported that lesion identification was nearly identical between the two modalities, with T1-weighted turbo spin-echo (TSE) performing better than CT or T1-weighted Dixon in-phase MRI.
In another study, PET/MRI detected all 48 bone metastases, whereas PET/CT detected only 45 (94%). The paper credited hyperintensity on T2-weighted images and increased FDG uptake for PET/MRI's superior results.
In another retrospective study, PET/MRI was superior by detecting bone involvement in more patients and more individual bone lesions.
Lung cancer
In this application, the researchers reviewed six studies with 194 patients who had non-small cell lung cancer or lung nodules. PET/MRI was found to have comparable accuracy to PET/CT, due primarily to FDG-PET's contribution of glucose metabolic information to both modalities. PET/CT and PET/MRI also had comparable accuracy for tumor, node, and metastasis (TNM) staging.
One study of 66 patients found high tumor stage concordance between PET/CT and PET/MRI, while three other papers concluded that the two modalities were equally proficient in assessing lymph node involvement and distant disease. PET/CT was "superior for lung nodule detection, but PET/MRI was equivalent for characterization of pulmonary lesions in a patient-based analysis," the authors added.
The final word
In summary, the authors wrote that PET/MRI protocols "are feasible across all types of cancer. Clear diagnostic advantages of PET/MRI, when used mainly for providing the anatomic framework, have not been established and will be difficult to demonstrate given the high accuracy of PET/CT."
They reiterated that PET/MRI is an "expensive technology that should not be used simply to replace PET/CT," and they recommended that additional comparative studies be performed between the two modalities to determine which protocols may yield the best results.
Spick said that PET/MRI still has "an interesting future," with an overall goal of determining the clear advantages of PET/MRI, including which functional MRI sequences will improve cancer assessment and which combination of different PET radioligands should be used.