Patients with a normal stress test but evidence of calcium in coronary arteries on PET/CT scans are not immune from a serious adverse cardiac event within a year, according to a study presented on Monday at the American Heart Association (AHA) annual meeting in New Orleans.
Researchers from Intermountain Medical Center Heart Institute in Salt Lake City found that 5% of patients who had moderate, severe, or very severe levels of calcium soon had a heart attack or stroke or died -- despite no evidence of blockage on stress tests.
"This is a clinically impactful study," lead author Viet Le, a physician assistant at Intermountain, told AuntMinnie.com. "It allows us to inform ourselves as clinicians and our patients who are at the highest level of risk for a cardiac event. Doing a functional test alone only tells us what is going on that day."
False confidence
Le said there is considerable concern among healthcare providers about patients who leave facilities with a false sense of security after a stress test finds no obstructions in the coronary arteries.
 Viet Le from Intermountain Medical Center Heart Institute.
Viet Le from Intermountain Medical Center Heart Institute."They go away thinking, 'I am invincible; I don't have any coronary disease; I can continue to eat what I eat, stay sedentary, and smoke,' " he said. "With a calcium scan, we see [patients] have already developed plaque, which causes coronary disease. It has been there long enough for calcium to settle inside the plaque."
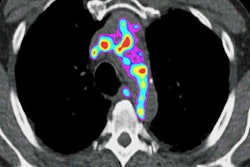
Indeed, clinicians know that calcium caused by plaque is a key indicator of heart disease. However, SPECT, the most widely used modality to image calcium, can expose patients to an excess amount of radiation. That issue is part of the reason why Intermountain installed its PET/CT scanner four years ago.
"With cardiac PET, we are finding that it has so much more accuracy than SPECT, which we were using," Le said. "Cardiac PET provides so much more for so much less radiation exposure, and with CT we can get anatomical imaging on a scanner that also gives us functional imaging."
The researchers started with a cohort of some 1,000 patients, one-third of whom had an abnormal stress test and were referred immediately for a follow-up procedure. The remaining 658 patients (average age, 67.2 ± 10 years) underwent a clinically indicated regadenoson rubidium-82 PET/CT scan and concurrent coronary artery calcification quantification between March 2013 and April 2015.
Calcium presence and density are measured through an Agatston score. The American College of Cardiology and the AHA consider a score of 300 or more as severe density.
For this study, the researchers classified an Agatston score between 0 and 10 as mild calcium, 11 to 299 as moderate, and 300 to 1,000 as severe. Scores greater than 1,000 were ruled as very severe. Segmented categories were used because patients' calcium levels change over time.
"People continue to gather more plaque after a score of 300," Le said. "Just saying greater than 300 lumps everyone in one group. There is a big difference above 1,000."
Calcium connection
In reviewing the 658 patients with normal stress tests and an indication of calcium, Le and colleagues found that 31 (5%) experienced a heart attack, stroke, or death within 12 months.
| Major adverse cardiac events (MACEs) by coronary artery calcium (CAC) score | ||
| CAC score category | No. of patients | Percent with MACE |
| None/mild (0-10) | 33 | 0% |
| Moderate (11-299) | 309 | 3.88% |
| Severe (300-1,000) | 190 | 5.26% |
| Very severe (> 1,000) | 126 | 7.14% |
Although the percentage of patients with major adverse cardiac events rose with CAC score, the trend fell just short of statistical significance (p = 0.058), Le said. By continuing this research and adding to the number of subjects, the group hopes to achieve that statistical significance.
In other findings, of the 17 men and 14 women who had a subsequent major cardiac event, 12 (38%) had a moderate level of calcium, 10 (31%) had severe calcium, and nine (30%) were in the very severe calcium group. There were no adverse cardiac events reported among the 33 patients with a normal stress test and no or only mild calcium levels.
While calcification cannot be reversed, the plaque that causes calcification can at least be stabilized with proper medication, diet, and exercise, Le said. In future studies, the researchers want to better determine if calcium can be used to identify and assess patients at risk for future adverse cardiac events, and whether the chances of such an outcome could be reduced.