CHICAGO - With high specificity and negative predictive value, FDG-PET/CT can accurately detect distant metastases in women with cervical or endometrial cancer and spare them from unnecessary aggressive therapy, according to a study presented on Sunday at RSNA 2016.
FDG-PET/CT also achieved a false-positive rate of less than 5%, prompting researchers to recommend that the hybrid modality be included as part of pretreatment evaluation for this patient population.
"At the time of diagnosis when the surgeons and medical oncologists are trying to formulate a treatment strategy, the performance of a single PET/CT gives much meaningful information in guiding where the likely sites of disease and distant metastases are," said lead author Dr. Michael Gee, PhD, a radiologist in abdominal imaging at Massachusetts General Hospital (MGH). "Having both benefits in a single imaging study is crucial in this population in terms of setting up the treatment strategy going forward."
ACRIN/GOG trial
The findings come from a secondary analysis of a clinical trial (ACRIN 6671/GOG 0233) jointly sponsored by the American College of Radiology Imaging Network (ACRIN) and the Gynecologic Oncology Group (GOG).
 Dr. Michael Gee, PhD, from MGH.
Dr. Michael Gee, PhD, from MGH.Gee and colleagues focused on women who had cervical or endometrial cancer and known lymph-node metastases in their abdomen or pelvis. These patients face potentially extensive radiation therapy and a dubious prognosis depending on the stage of the disease and lymph-node involvement.
"The original purpose of the trial was to evaluate PET/CT for the ability to detect lymph-node metastases in women with high-risk endometrial and locoregionally advanced cervical cancer," Gee told AuntMinnie.com. "Both of these cancers at these stages are amenable to surgical resection with adjuvant therapy, but we also know that patients with known lymph-node metastases do worse overall from a prognostic point of view."
The current standard for staging lymph nodes is through surgery, which is not without risk. Gynecological surgeons must dissect every lymph node, which is a laborious task. A hard-to-reach location can extend exploratory surgery, and physically removing the lymph nodes occasionally is associated with morbidity and other complications.
"Being able to diagnose lymph-node metastases without surgical dissection on every lymph node is helpful for the surgeons, so they can know ahead of time which lymph nodes to go after to get histological confirmation," added Gee, who also serves as chief of pediatric radiology at MGH and as an associate professor of radiology at Harvard Medical School.
Patient benefits
The study presented at RSNA included 153 cervical cancer patients with a mean age of 48.9 years (range, 24-74 years) and 203 endometrial cancer patients with a mean age of 62.7 years (range, 36-81 years) from 28 different sites.
Two central readers were blinded to results from the sites and reference standards. The pair evaluated FDG-PET/CT scans for distant metastasis on a scale of 1 to 6, with 4 to 6 indicating a positive finding. Pathology and follow-up radiology reports were used as the reference standards.
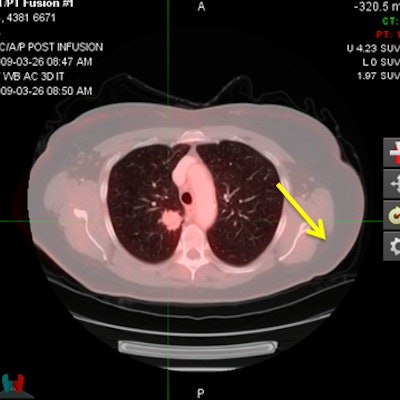
FDG-PET/CT revealed distant metastases in 21 (13.7%) of the cervical cancer patients and in 24 (11.8%) of the endometrial cancer patients. The most common locations for distant metastases among women with cervical cancer were the lungs (5.2%) and the peritoneum (4.6%). Among the endometrial cancer patients, the peritoneum (6.4%) was the most common site for distant metastases.
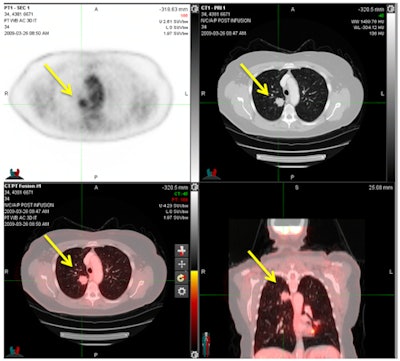 FDG-PET/CT shows a pulmonary metastasis in a cervical cancer patient. PET (upper left), CT (upper right), and PET/CT (bottom row) demonstrate an FDG-avid nodule in the right lower lobe consistent with a pulmonary metastasis and confirmed by histology. Image courtesy of Dr. Michael Gee, PhD.
FDG-PET/CT shows a pulmonary metastasis in a cervical cancer patient. PET (upper left), CT (upper right), and PET/CT (bottom row) demonstrate an FDG-avid nodule in the right lower lobe consistent with a pulmonary metastasis and confirmed by histology. Image courtesy of Dr. Michael Gee, PhD.The two readers collectively achieved excellent results in terms of specificity and negative predictive value for both cervical and endometrial distant metastases.
| FDG-PET/CT results for both readers | |||||
| Cervical cancer metastasis | Endometrial cancer metastasis | ||||
| Sensitivity | 47.6% | 66.7% | |||
| Specificity | 93.9% | 93.9% | |||
| Negative predictive value | 91.9% | 95.5% | |||
| Positive predictive value | 55.6% | 59.3% | |||
| Area under the receiver operating characteristic curve | 0.75 | 0.84 | |||
"In summary, greater than 10% of advanced cervical and high-risk endometrial cancer patients have unsuspected distant metastases at the time of presentation," Gee told RSNA attendees. "FDG-PET/CT demonstrates high accuracy and negative predictive value for distant metastases, and we believe it should be included in the staging evaluation of these patients."
Need for collaboration
There also was "very good correlation" between FDG-PET/CT and histological confirmation of distant metastases, which emphasizes the need for radiologists and surgeons to have a close relationship when interpreting the images and locating the distant metastases.
"The clinical trial mandated a joint review of the PET/CT findings between the radiologist and the surgeon prior to the operation," Gee said. "This part of the study is a good lesson for caregivers -- that there is such a close link between imaging findings and what surgeons observe directly in the operating room."
Given the results, Gee recommended that FDG-PET/CT be used in combination with histological confirmation to triage these two patient populations into systemic therapies if distant metastases are present, as well as to help avoid the morbidity associated with unnecessary locoregional-directed treatments.




















