By adding a time-of-flight (TOF) technique to pediatric PET scans, clinicians can adjust radiation dose levels by as much as 50% with no discernible loss of diagnostic image quality, according to a study presented at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting in Philadelphia.
Researchers from Children's Hospital of Philadelphia (CHOP) and the University of Pennsylvania (UPenn) found that while the visual image quality can degrade noticeably in low-dose images, a maximum radiation dose reduction of 50% can still produce sufficient diagnostic images.
"Patient safety remains very critical. Mostly that means minimizing exposure to radiation," said lead investigator Jeffrey Schmall, PhD, a research associate in UPenn's department of radiology. "Our study demonstrates that dose reduction is feasible for pediatric patients without degrading the diagnostic quality when using TOF PET/MRI."
Radiation concerns
For pediatric patients, avoiding unnecessary radiation exposure is paramount: Their sensitivity to radiation is heightened because of their age and the potential for repeat imaging scans. Even when young patients are cured of their disease, there is a greater risk of radiation-induced cancers because of the many years left in their lifespan, the authors noted.
 Jeffrey Schmall, PhD, from the University of Pennsylvania.
Jeffrey Schmall, PhD, from the University of Pennsylvania.Beyond the radiation dose issue, identifying metastatic liver lesions can be a challenge with FDG-PET because high organ background uptake and abdominal photon attenuation locally reduce image contrast.
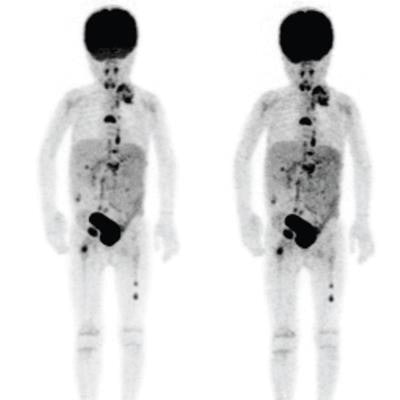
CHOP's recently constructed Buerger Center houses the hospital's PET/MRI system (Signa PET/MR, GE Healthcare), which was installed in December 2016. Since then, clinicians have imaged more than 130 pediatric patients with the hybrid imaging device.
With PET scans, radiation dose depends primarily on injection activity. Clinicians at CHOP use a linear, weight-based injection regimen based on minimum and maximum recommended guidelines. There still remains, however, a "wide range in the variability of injection regimens, probably due to patient variability but also variability in PET scanner performance," Schmall said.
With non-TOF PET, the signal-to-noise ratio is proportional to the number of detected counts. When scan time and injection activity are set, the number of counts is based on the number of decays in the body multiplied by the efficiency of the scanner. With TOF PET, TOF helps localize each detected event based on the diameter of the imaged object and time-of-flight image resolution, Schmall explained.
"Mathematically, it has been shown that TOF localization reduces the statistical noise in the reconstructed image in a way similar to increasing the number of detected events," he said. "This effect has been well-demonstrated in FDG-PET of adult populations and is typically used to reduce scan time and increase patient throughput."
Scanner performance
As for variability in performance between different PET scanners, there is a fivefold difference in photon sensitivity between CHOP's PET/CT system (Gemini 16, Philips Healthcare) and its PET/MRI system. When the time-of-flight sequence is added, a huge difference in signal-to-noise ratio and the number of detected counts can be expected, Schmall said.
"So the question is: Do we match the signal-to-noise ratio, which could potentially allow us to lower the dose by a factor of five or maybe 10?" he said. "Or do we keep the same dose and increase the image signal-to-noise ratio and perhaps improve the diagnostic performance of the scanner? Understanding this relationship between PET scanner performance and image quality becomes a central question."
In this retrospective study, the researchers selected FDG-PET images of metastatic liver lesions acquired between December 2016 and December 2017. Liver images were chosen because of the high background uptake and uniform distribution. Several different diseases were included in the analysis, such as lymphoma and medulloblastoma.
The PET/MRI protocol used included T1-, T2-, and diffusion-weighted MRI, along with three-minute PET imaging per bed position. In all, there were 12 PET scans from 11 patients who had an average age of 12 years (range: 2-19 years) and an average weight of 75 lb (range: 40-108 lb). There were 28 lesions in the final analysis, with an average size of 1.2 cm (range: 0.6-2.5 cm). Lesion standardized uptake value (SUV) ranged from 2.3 to 7.8, with an average of 4.7.
Image reconstruction
Schmall and colleagues then generated TOF PET images, beginning with a full dose of 3.7 MBq/kg and continuing with reduced dose levels of 50%, 33%, 22%, and 11% (0.4 MBq/kg). They also recorded background measurements of the liver for maximum standardized uptake values (SUVmax) and mean SUV for eight volumes of interest (VOIs).
Two radiologists were asked to determine the number of lesions detected only on PET and with fused PET/MRI to evaluate PET image quality at various dose levels. As the images were presented randomly, the readers were also asked to provide a confidence level.
In reviewing the results, the researchers found that the variability of FDG uptake and SUVmax increased in healthy liver tissue as simulated dose levels decreased. For patients between 1 and 5 years old, FDG-avid liver lesions at half dose showed a 6% increase in SUVmax; there was a 14% increase at one-third dose. SUVmean, meanwhile, remained relatively stable even at the lowest doses.
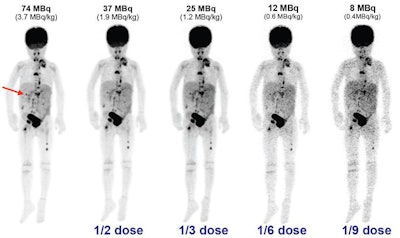 Maximum intensity projection (MIP) images from a 4-year-old patient highlight (arrow) one of three lesions. Researchers reconstructed TOF PET images down to 11% of the standard dose. While the image quality worsens, lesion conspicuity remains relatively stable at one-third the dose. Images courtesy of Jeffrey Schmall, PhD.
Maximum intensity projection (MIP) images from a 4-year-old patient highlight (arrow) one of three lesions. Researchers reconstructed TOF PET images down to 11% of the standard dose. While the image quality worsens, lesion conspicuity remains relatively stable at one-third the dose. Images courtesy of Jeffrey Schmall, PhD.The two readers expressed no strong preference for higher dose images, nor did they see any significant degradation in diagnostic image quality at as low as one-third the dose (1.2 MBq/kg).
Of 23 diagnostically confirmed lesions, one reader identified all of the lesions at full dose but 25 lesions at half dose and 23 lesions at one-third dose. The second reader detected 19 lesions at both full and half dose and 18 lesions at one-third dose.
So how should these results be interpreted? Even with the accuracy of SUV uptake maintained down to one-third dose, visual image quality "noticeably degrades for low-dose images, and based on our reader studies, a maximum dose reduction of half is suggested," the researchers wrote.
Schmall and colleagues plan to use the findings to develop new imaging protocols and injected activity regimens at CHOP to reduce radiation exposure among pediatric patients.
"We will look at adjusting clinical protocols to about 30% of dose reduction (to 2.6 MBq/kg), and potentially up to a 50% reduction in high-risk patients (to 1.8 MBq/kg)," he said.




















