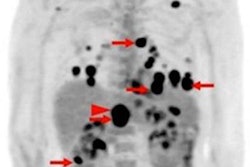
FDG-PET/CT scans can predict the success of radiation therapy in patients with spinal metastases, especially in regard to progression-free survival, according to a study published online September 28 in PLOS One.
Patients with a reduction of more than 70% in maximum standardized uptake values (SUVmax) on PET/CT scans obtained before and after treatment had better progression-free survival than patients below that mark, researchers found.
"With advances in oncology and the successful treatment of metastatic spinal cord tumors, we expect patients with spinal metastases to live longer," wrote South Korean researchers led by Dr. Jinhyun Choi from Yonsei University College of Medicine. "Consequently, a method is required that can estimate their expected survival and help in the selection of successful treatment."
The researchers retrospectively analyzed 42 patients (median age, 58 years; range: 24-80 years) with spinal metastases who received radiotherapy from January 2010 to December 2014. The most common primary cancer was located in the breast among 18 patients (43%), followed by hepatobiliary cancer with 10 cases (24%).
All patients had FDG-PET/CT scans before and after treatment, with changes in metabolic responses measured by maximum, mean, and peak standardized uptake values (SUVmax, SUVmean, and SUVpeak), as well as metabolic tumor volume and total lesion glycolysis. Those variables were then correlated with the patients' clinical outcomes.
The researchers found that radiotherapy produced significant decreases in SUVmax, SUVmean, SUVpeak, and total lesion glycolysis (p < 0.001), compared with baseline values. The change in metabolic tumor volume was not statistically significant.
| PET/CT imaging in patients with spinal metastases | |||
| Pretreatment | Post-treatment | p-value | |
| Mean SUVmax | 6.87 | 2.99 | < 0.001 |
| Mean SUVmean | 2.27 | 1.41 | < 0.001 |
| Mean SUVpeak | 5.75 | 2.33 | < 0.001 |
| Mean metabolic tumor volume | 12.06 | 12.04 | 0.976 |
| Mean total lesion glycolysis | 52.84 | 24.17 | < 0.001 |
After radiation therapy, the patients' median progression-free survival was 15 months and median overall survival was 22.4 months.
Twelve subjects (29%) experienced local progression after radiation therapy. The only potential predictor of local disease progression was a reduction in SUVmax, the researchers found.
In addition, patients whose SUVmax dropped by more than 70% between the pretreatment and post-treatment scans had better progression-free survival. All nine patients with more than a 70% reduction in SUVmax experienced two-year progression-free survival; in comparison, of the 33 patients who did not achieve that SUVmax mark, only 64% achieved two-year progression-free survival (p = 0.036).