FDG-PET/CT scans can help detect major depression in cancer patients, according to research published May 6 in PLOS One. The finding suggests PET/CT images could serve double duty by helping screen for major depression in cancer patients.
Researchers found a link between metabolic activity in the brain and depression among patients with multiple myeloma, according to Dr. Xiaofei Wang and colleagues at the University of Arkansas for Medical Sciences in Little Rock.
"The study demonstrated that the major depression group had a significant reduction of metabolic activity as compared to the nonmajor depression group at the global level," Wang et al wrote.
Previous PET studies have shown decreased glucose metabolism in the prefrontal, insular, and limbic cerebral areas of the brain in patients with major depression. Major depression affects approximately one in four cancer patients and frequently compromises cancer treatments; it can increase mortality rates by up to 39%.
Moreover, oncology clinics lack practical, objective tools for simultaneous evaluation of cancer and major depression, according to the authors. The success of traditional questionnaires for psychological evaluation highly depends on professional experience and communication skills to make patients willing to share their feelings. An objective, reliable, and measurable method ideal for assessing a cancer patient's mental status would be ideal, they stated.
In this study, the researchers sought to perform a retrospective analysis of whole-body FDG-PET/CT images to identify brain regional metabolic patterns of major depression in multiple myeloma patients. They included 134 multiple myeloma patients, 38 with major depression and 96 without major depression, from the university's FDG-PET/CT imaging database from 2010 to 2019. Whole-body PET/CT scans were performed after approximately 60 minutes of uptake.
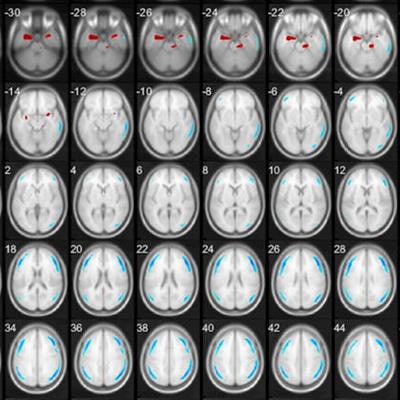
Based on a height threshold criteria of T = 4.38 and an extent threshold > 100 voxels, statistic parameter mapping demonstrated that the major depression patient group had significant regional metabolic differences (clusters of continuous voxels) as compared with the group without major depression. Five significant hypo- and three hypermetabolic clusters from CT contrast maps were localized on glass-brain view and were consistent with previously published brain metabolic changes in major depression patients, the authors reported.
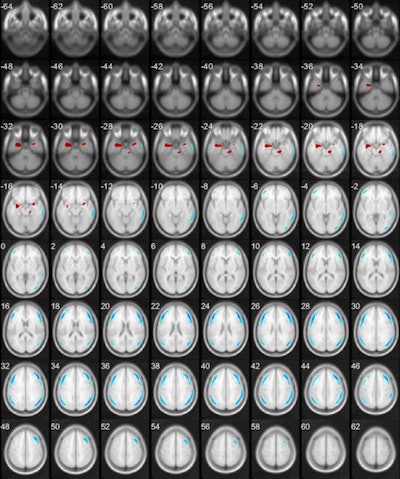 A map of significantly changed metabolic clusters in patients with major depression as compared with the control. Statistical parametric maps displayed on transverse sections depicting regions of hypermetabolic (red) and hypometabolic (blue) changes (Image courtesy of Plos One).
A map of significantly changed metabolic clusters in patients with major depression as compared with the control. Statistical parametric maps displayed on transverse sections depicting regions of hypermetabolic (red) and hypometabolic (blue) changes (Image courtesy of Plos One).In addition, having identified these fingerprinting clusters as classification features for major depression, the researchers fed the data through two artificial intelligence algorithms to assess them as predictive models for screening major depression among multiple myeloma patients. Using machine-learning algorithms to identify the presence of major depression in multiple myeloma patients with FDG-PET/CT was another first, the authors noted.
Two machine-learning models stood out, with performances of 85.1% accuracy, 79% sensitivity, and 88% specificity compared with previous resting-state fMRI and perfusion SPECT machine learning studies in large sample groups.
A machine-learning algorithm would not replace the need for a psychological evaluation, but it could serve as an alert for clinicians that metabolic changes in the patient's brain may be associated with depression, the researchers suggested.
"The eventual progression of these methods is to screen all patients undergoing PE/CT for major depression. With the rapid advancement of AI, there is potential for automated screening of patients during the staging of PET/CT for major depression, and this may increase awareness and identification of patients needing additional support for depression," they concluded.