Are ventilation nuclear medicine lung scans really needed in cases of suspected pulmonary embolism (PE)? Perhaps not, according to two student talks on June 11 at the annual meeting of the Society of Nuclear Medicine and Molecular Imaging (SNMMI).
Motivated by limitations on ventilation studies during the COVID-19 pandemic, researchers from Saint Louis University found that SPECT/CT perfusion studies were up to the job of assessing for PE. Meanwhile, researchers from Froedtert and Medical College of Wisconsin concluded that PE could be safely ruled out in four out of five patients based just on perfusion-only lung scans.
Nuclear medicine ventilation/perfusion (V/Q) lung scans have traditionally been used to assess for PE. Early on in the pandemic, however, the SNMMI published guidance that discouraged use of ventilation on lung scans, leading many hospitals to switch to a perfusion-only protocol. That model made it difficult to rule out PE for everyone, according to Jacob Whipple of Saint Louis University. The SNMMI guidance was later updated in September 2020 and again in March.
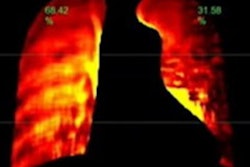
As an alternative to the traditional V/Q lung scan, SPECT/CT perfusion studies show both anatomical and physiological data. They can also be easily completed with little to no patient discomfort, Whipple said.
"It also uses some of the newest technology," Whipple said.
As a result, the researchers sought to determine if SPECT/CT lung perfusion studies could provide radiologists with enough information to accurately conclude if patients have a PE. Their study included 43 cases from St. Louis University Hospital, two of which were positive for PE and one of which was indeterminate.
Whipple shared several cases, including a SPECT/CT exam performed on a 70-year-old woman, that showed the modality was beneficial in diagnosing thromboembolic pathologies and also helpful in showing other CT findings.
Based on their experience, "SPECT/CT is proven to be beneficial and sufficient in ruling out PE, but more data may be necessary to add to these conclusions," Whipple said. "At this point, physicians at Saint Louis University Hospital feel that SPECT/CT gives just as much information as ventilation, if not more."
SPECT/CT could also possibly take less time to perform, he said. In addition, other research studies at Saint Louis University Hospital are investigating the impact of this approach on radiation dose to both the patient and the technologist, Whipple said.
"The hospital will continue to perform the SPECT/CT perfusion as their exam of choice, even though the [SNMMI] may [now] deem ventilation to be safe," he said. "This means that more information will continue to be collected and the radiologists are confident in their SPECT/CT protocol for lung pathology. They find this to be sufficient in differentiating pulmonary emboli from other pathologies."
Ventilation scans not needed?
After reviewing perfusion-only nuclear medicine lung scans performed during the COVID-19 pandemic at their institution, researchers from Froedtert and the Medical College of Wisconsin concluded that ventilation scans wouldn't be needed to confidently rule out PE in most cases.
The researchers led by Lauren Brickley randomly selected 180 patients over a seven-month period who had received a perfusion-only lung scan for the indication of suspected PE. After reviewing the patient results from the electronic medical record, the radiologists' impressions were classified into four groups:
- Normal/Very-low probability of PE: 72 (40%)
- Low probability of PE: 73 (40%)
- Indeterminate/Intermediate probability of PE: 30 (17%)
- High probability of PE: 5 (3%)
As a result, the perfusion-only images indicated a very low or low probability of PE in 80.6% of patients, therefore ruling out PE without the need for ventilation images, she said. The 19.4% of patients who showed an intermediate or high probability of PE would benefit, however, from a ventilation lung scan to confirm that the defects shown on the perfusion scan are in fact due to a PE.
"Overall, this means that without the limits on aerosol-generating procedures during the COVID-19 pandemic, ventilation scans could have been obtained on that 19% of patients that were in the intermediate or high-probability group, giving more information and helping to rule in or out pulmonary embolism," Brickley said. "This type of a protocol ensures that patients are receiving accurate results with the most appropriate and comfortable imaging protocol for each patient individually."