Tau PET is superior to amyloid PET and MRI for detecting cognitive decline in Alzheimer's disease patients over time and may serve as a prognostic tool to help manage patients in the early stages of the disease, according to a study published June 28 in JAMA Neurology.
In a large multicenter prognostic study, a group of Swedish, South Korean, and U.S. researchers examined the accuracy of flortaucipir F-18 and RO948 F-18 PET for detecting tau pathology in patients with Alzheimer's disease dementia, mild cognitive impairment, and normal cognition. The team found the radiotracers performed significantly better in all groups at predicting cognitive changes when compared head-to-head against MRI and amyloid PET imaging.
The authors found that tau PET could be an essential prognostic tool for people with Alzheimer's disease to help patients and their families plan for the future, increase safety, and optimize medical decisions regarding their care.
"These findings suggest that tau PET is a promising prognostic tool for predicting cognitive decline in preclinical and prodromal stages of Alzheimer disease," wrote lead author Rik Ossenkoppele, PhD, of the Clinical Memory Research Unit at Lund University in Malmö, Sweden.
Flortaucipir F-18 was approved by the U.S. Food and Drug Administration in May 2020 for adult patients with cognitive impairment who are being evaluated for Alzheimer's disease. RO948 F-18, a derivative of flortaucipir F-18, is being tested in late-stage clinical trials. Despite these developments, accurately predicting rates of cognitive decline in individuals with Alzheimer's disease remains challenging, the authors noted.
In this study, Ossenkoppele and colleagues assessed the prognostic accuracy of baseline flortaucipir F-18 and RO948 F-18 PET for detecting tau pathology in individuals across the Alzheimer disease clinical spectrum and compared the tracers against established MRI and amyloid PET markers.
The study included 1,431 participants enrolled in ongoing, international studies between June 2014 and February 2021. The mean age of the study participants was 71.2 years; of the study cohort, 47.5% were women and 52.5% were men. In addition to tau PET, all participants underwent a medical history assessment and neurological examination, MRI, and a neuropsychological test, the Mini-Mental State Examination (MMSE).
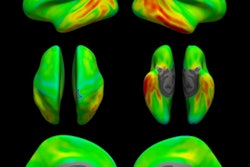
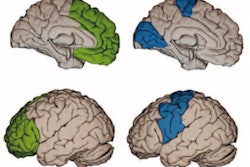
The investigators used the measures of baseline flortaucipir F-18/RO948 F-18 PET retention within a temporal region of interest, MRI-based Alzheimer's disease-signature cortical thickness, and amyloid PET centiloids -- along with models adjusted for age, sex, education, and cohort -- to predict changes in the MMSE. They assessed performance using R2 values, a statistic that describes how well a model fits the task.
Ossenkoppele and colleagues found that flortaucipir F-18 uptake predicted longitudinal changes in MMSE. This uptake effect was stronger than for Alzheimer's disease-signature cortical thickness and amyloid PET across all participants, including the amyloid-positive group with mild cognitive impairment and the amyloid-positive group who were not cognitively impaired.
|
Association of baseline tau PET, MRI, and amyloid PET with change over time in mini-mental state examinations (R2 values) |
|||
| Cohort | Amyloid PET | MRI | Flortaucipir F-18 PET |
| All participants (n = 1,431) | 0.17 | 0.24 | 0.35 |
| Amyloid-positive mild cognitive impairment group (n = 271) | 0.07 | 0.15 | 0.25 |
| Amyloid-positive cognitively impaired group (n = 253) | 0.08 | 0.08 | 0.16 |
The findings were replicated in the RO948 F-18 PET cohort, the group noted.
Altogether, the study results are consistent with those of a recent cross-sectional study showing that tau PET is more sensitive than MRI for detecting early cognitive change. However, at the dementia stage, tau PET and MRI perform more equally.
"Our findings suggest that although tau PET as a diagnostic marker is most valuable at the dementia stage of [Alzheimer's disease], the optimal time window for tau PET as a prognostic marker is during the prodromal and preclinical stages of [Alzheimer's disease]," the researchers concluded.