SPECT scans of patients hospitalized for heart failure can help predict their risk of further life-threatening events after they are discharged, according to a study published October 13 in JACC: Cardiovascular Imaging.
Japanese investigators at Osaka University analyzed data from heart failure patients who underwent iodine-123 metaiodobenzylguanidine (I-123 MIBG) SPECT scans. They found patients with higher levels of blood-flow defects on SPECT scans were significantly more at risk of dying from cardiac events than those with low levels.
"I-123 MIBG-SPECT data accurately identified subjects who were at risk of poor outcomes because of cardiac causes," wrote first author Dr. Masahiro Seo, a cardiologist at Osaka General Medical Center, and colleagues.
Recognizing patients in these settings is important to prevent readmissions because of heart failure, the authors wrote.
Determining how much blood the heart's left ventricle pumps out with each contraction (left ventricle ejection fraction, or LVEF) is a cornerstone for identifying patients at risk of sudden cardiac death. As LVEF declines, often due simply to age, the risk of death increases.
Patients in this study had been diagnosed and hospitalized for heart failure with "preserved" ejection fraction (HFpEF), which occurs when the left ventricle can pump well but may be stiff so that it cannot relax and fill with blood as well as normal.
"The precise risk stratification of patients with HFpEF is clinically relevant for physicians to optimize medicine and prevent adverse outcomes," the researchers wrote.
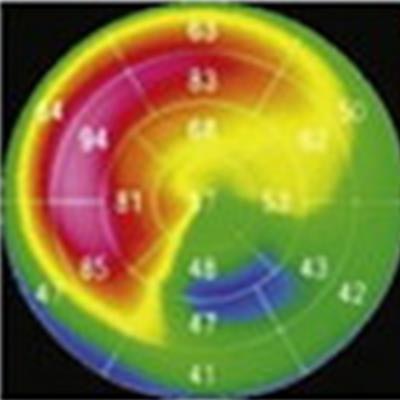
I-123 MIBG-SPECT imaging measures the activity of nerve cells in the heart muscle, which may be overstimulated to compensate for defects in blood flow. The "uptake" of 1-123 MIBG by stimulated nerve cells is visible on SPECT images. Yet no information is available on the prognostic value of cardiac I-123 MIBG-SPECT in patients with HFpEF, according to the authors.
In this prospective study, Seo and colleagues studied data on 148 patients admitted with HFpEF who underwent cardiac I-123 MIBG-SPECT imaging (BrightView, Philips Healthcare) prior to discharge from the hospital. They measured the uptake of I-123 MIBG in 17 regions of the left ventricle of the patients and then calculated an average total defect score by adding the scores of each of the 17 segments.
All of the patients in the study had follow-ups at least every one or two months for an average of 2.4 years. During the follow-up period, 61 patients experienced cardiac events: 49 patients died, including 23 cardiac deaths. Fifty-three patients experienced emergent heart failure hospitalization.
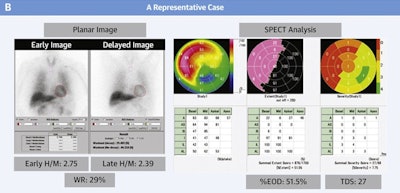 A representative case: an 83-year-old female patient had high total defect score and high percent extent of dysinnervation (% EOD) despite high late heart-to-mediastinum ratio (H/M) of ≥ 1.9. She experienced emergent heart failure hospitalization 11 months after discharge. Image courtesy of JACC: Cardiovascular Imaging.
A representative case: an 83-year-old female patient had high total defect score and high percent extent of dysinnervation (% EOD) despite high late heart-to-mediastinum ratio (H/M) of ≥ 1.9. She experienced emergent heart failure hospitalization 11 months after discharge. Image courtesy of JACC: Cardiovascular Imaging.The analysis revealed total defect scores on I-123 MIBG-SPECT were significantly associated with cardiac events. Patients with high total defect scores had a significantly greater risk (63%; hazard ratio [HR], 4.69) of cardiac events than those with middle (40%; HR, 2.46) or low (20%; HR, 1.0) total defect scores, the authors found.
"These results indicate that obtaining I-123 MIBG-SPECT analysis would provide additive prognostic value in patients with HFpEF," they wrote.
The researchers noted studies show the prevalence of heart failure in patients with HFpEF is rapidly increasing and carries a high economic burden worldwide. This is the first study to demonstrate the prognostic significance of cardiac I-123 MIBG-SPECT imaging in nonischemic heart failure patients with preserved LVEF and suggest adding I-123 MIBG-SPECT findings to conventional imaging could improve risk stratification in patients, they added.
"Further investigation on the therapeutic implication targeting cardiac sympathetic nerve dysfunction in HFpEF is warranted," Seo and colleagues concluded.





















