Patients with neurological symptoms due to COVID-19 appear to be in the clear after five months, according to a study presented Monday morning at RSNA 2021 in Chicago.
An Italian group led by Anna Lisa Martini of the nuclear medicine unit at the University of Florence looked at FDG-PET scans in patients up to nine months after they were infected and found initial brain hypometabolism associated with neurological impairment returned to normal at five months.
"Cortical functional impairment observed in neuro-SARS-CoV-2 patients is likely to be transient and almost reversible, and possibly due to synergistic effects of systemic virus-mediated inflammation," Martini said.
Clinical reports indicate that the SARS-CoV-2 virus has neuroinvasive potential. Several hypotheses have been proposed to explain the pathophysiologic mechanisms underlying central nervous system (CNS) involvement, but the effects on the brain are unclear, Martini said.
In this study, Martini and colleagues aimed to characterize time-dependent brain functional impairment in SARS-CoV-2 patients with newly originated neurological symptoms and to suggest physiopathology mechanisms underlying CNS involvement.
The group enrolled nine patients with neuro-SARS-CoV-2 and new onset neurological cognitive disturbances. Patients reported symptoms that included disorientation, altered mental status, headache, agitation delerium, and somnolence. Patients underwent baseline FDG-PET scans during the acute phase of infection. Patients then underwent scans at one, two, three, five, seven, and nine months later.
The researchers analyzed brain metabolism using an optimized and validated voxel-based statistical parametric mapping method at the single-subject level (p = 0.01) based on comparisons with a large and well-selected healthy control dataset.
Clinical findings from an extended neurophsychological test battery showed that at three months, four patients began to show improvement from initial declines during the acute phase of infection in memory and executive functions. At five months, the patients showed progressive improvement in memory and executive function, with some reported episodes of frontal headache.
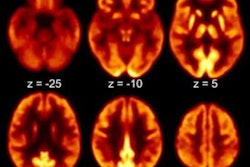
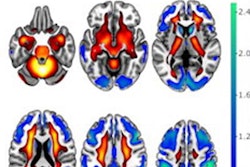
Molecular imaging findings in five patients with FDG-PET scans within two months from the infection showed extended orbital, prefrontal, and temporal-parietal cortex hypometabolism. Three patients with FDG-PET scans five months after the SARS-CoV-2 acute phase showed normal brain metabolism and normal cognitive scores.
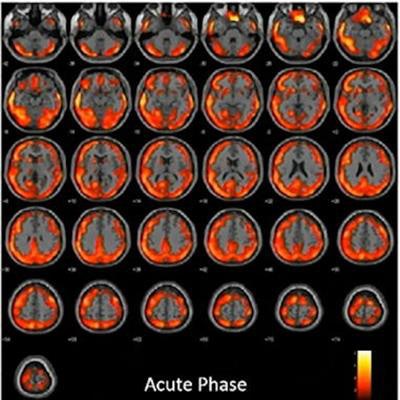
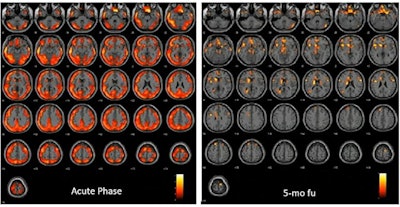 In one patient, FDG-PET during the acute phase showed an extended and severe hypometabolism affecting almost all brain cortices and some subcortical regions (caudates and L-thalamus). At five-month follow-up, only some spots of hypometabolism are present in the superior and middle frontal cortex, superior medial frontal cortex, and L-caudate nucleus. Image courtesy of Anna Lisa Martini.
In one patient, FDG-PET during the acute phase showed an extended and severe hypometabolism affecting almost all brain cortices and some subcortical regions (caudates and L-thalamus). At five-month follow-up, only some spots of hypometabolism are present in the superior and middle frontal cortex, superior medial frontal cortex, and L-caudate nucleus. Image courtesy of Anna Lisa Martini.The results demonstrate the following three key points, Martini explained.
- Patients with ongoing SARS-CoV-2 infection featured widespread hypometabolism affecting almost all brain cortices.
- Patients evaluated in post-SARS-CoV-2 infection phase presented with a rather extended cortical hypometabolism only close to the acute phase.
- Along with remission of clinical and cognitive symptoms, the brain hypometabolism reduces progressively as a function of time from acute phase.
Ultimately, the study is preliminary, but it establishes that an extended and severe cortical hypometabolism possibly also involving subcortical areas can be observed in patients during the acute phase of SARS-CoV-2 infection, Martini said.
"Along with remission of clinical neurological symptoms, such hypometabolism progressively reduces during time, especially after the third month from the acute phase," she concluded.