SPECT myocardial perfusion imaging may be a better approach than coronary angiography for predicting survival of patients after coronary artery bypass, according to a study published November 9 in The Annals of Thoracic Surgery
A group led by Dr. Ho Hwang, PhD, of Seoul National University Hospital in South Korea compared SPECT myocardial perfusion imaging (MPI) to coronary angiography for determining the success of coronary artery bypass graft surgery. They found SPECT MPI was better at predicting long-term outcomes in patients.
"Myocardial SPECT has several advantages, such as wide availability, noninvasiveness, and high diagnostic performance, in contrast to the limitations of [coronary angiography], such as its invasiveness and high cost," the group wrote.
Success after coronary artery bypass graft (CABG) surgery to treat coronary artery disease is measured by the "completeness" of revascularization after the procedure. The goal is the successful revascularization of all coronary artery lesions with significant stenosis. This stenosis is usually determined by the anatomic criteria, which depend on the results of angiography.
However, artery flow-limiting defects may also be evaluated on a functional molecular level in these patients by SPECT MPI, a noninvasive technique.
"To our knowledge, this is the first study to explore the impact of functional [complete revascularization], which is evaluated with myocardial SPECT, on long-term clinical outcomes after CABG," the authors wrote.
The researchers studied data on 1,162 patients who underwent off-pump coronary artery bypass graft surgery for three vessel disease and postoperative myocardial SPECT and angiography. Median follow-up duration was 82.4 months.
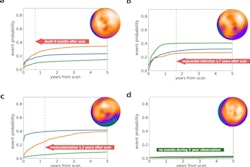
Of the total patient cohort, angiography identified complete revascularization in 87.3%, while SPECT imaging detected complete revascularization in 92.7%. Early mortality occurred in seven patients, while late death occurred in 322 out of 1,155 early survivors. The 5- and 10-year overall survival rates were 84.3% and 66.7%.
The researchers found that functional completeness of revascularization on SPECT was a statistically significant risk factor (p = 0.038), whereas anatomic completeness was not (p = 0.859).
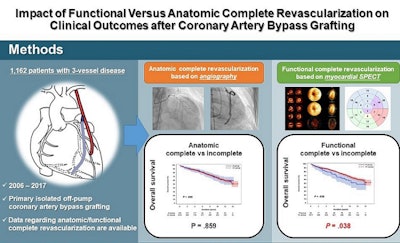 Image courtesy of The Annals of Thoracic Surgery.
Image courtesy of The Annals of Thoracic Surgery.The team did underscore that their study represents early research, and coronary angiography remains key to the overall assessments of coronary artery disease for surgical revascularization.