Hunting for the ideal contrast agent to use during intraoperative MR imaging, German neuroradiologists from the University of Heidelberg Medical School have reported encouraging results with MIONs, or monocrystalline iron oxide nanoparticles.
Unlike traditional paramagnetic contrast agents, MIONs do not appear to cause surgically induced intracranial contrast enhancement when they are administered. This non-tumorous contrast enhancement is brought on by surgical trauma, and can be a potential source of error, explained Dr. Michael Knauth and co-authors in the American Journal of Neuroradiology. In comparison, MIONs are taken up by tumor cells through endocytosis and then are eliminated from the blood by the reticuloendothelial system.
"One of the main indications for intraoperative MR imaging is the assessment of the radicality of surgical resection of brain tumors. However, surgical manipulation opens vessels and can cause blood-brain barrier disruption, which in turn causes surgically induced intracranial contrast enhancement. The basic idea of our study was that there is a window in which the MIONs are already completely eliminated from the blood…but are still stored in the brain," the authors wrote (AJNR, January 2001, Vol.22:1, pp.99-102).
Using animal models, the researchers tested MIONs on three different groups of rats. Group 1 consisted of 16 animals with different types of brain lesions. The animals were examined with a 1.5-tesla MR scanner and a paramagnetic contrast agent (Magnevist, Schering AG, Berlin). According to the results, "meningeal enhancement was seen in all animals regardless of the type of lesion inflicted on the brain. Intraparenchymal enhancement was also seen in all animals."
Group 2 was made up of 10 rats with different types of brain lesions. Each animal received an intravenous dose of 10 mg of MIONs per kilogram of body weight. In this group, MRI did not reveal preoperative intracranial hyperintensities.
"This indicated that the normal rat brain does not store MIONs in an amount detectable by MRI," they wrote.
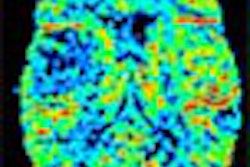
Finally, in Group 3, 10 animals with C6-glioma all underwent surgical resection, using the same MIONs dosage as in Group 2. In the final analysis, the tumors were depicted as hyperintense areas on preoperative T1-weighted images. The average contrast between tumor and normal brain tissue was 1.32.
"After administration of MIONs, malignant gliomas appear hyperintense on T1-weighted sequences…; this phenomenon lasts longer than 24 hours. This represents the window that might be used for intraoperative MR imaging because it might offer a means of detecting residual tumor without superimposed confusing surgically induced intracranial contrast," the authors said.
While MIONs do show promise, the group acknowledged that more research is needed. For example, it's not clear which intracranial tumors respond best to MIONs, as only malignant glioma models have been studied thus far. Also, the optimal dosage is still undetermined. The 10-mg dosage used in the study was based on preliminary research done by one of the co-authors, Dr. Thomas Egelhof, Knauth said.
Knauth wrote that the group is seeking permission to study MIONs in patients with high-grade gliomas.
In a separate study, researchers from the University of California, San Francisco experimented with an MR contrast agent currently in clinical trials, ultrasmall superparamagnetic iron oxide particles (USPIO).
A macromolecular substance, USPIO could potentially improve the characterization of individual tumors by defining their microvascular properties, the authors wrote in the latest issue of Radiology.
The group compared two macromolecular contrast agents -- albumin-(Gd-DTPA) and NC100150 injection (Clariscan, Nycomed Amersham Imaging, Princeton, NJ) -- in experimental breast tumors induced in an animal model.
A spectrum of breast tumors from fibroadenoma to anaplastic adenocarcinoma was induced in 19 rats. MR imaging was performed on a 2-tesla superconducting system (Omega CSI-II, Bruker Medical, Billerica, MA). Dynamic contrast-enhanced MRI was performed with a transverse gradient-recalled sequence. The two macromolecular contrast agents were used on sequential days.
"NC100150 injection consists of USPIO particles composed of single crystals (4-7-nm diameter) and stabilized with a carbohydrate polethylene glycol coat…the injection was administered at a dose of 1 mg of iron per kilogram, 24-30 hours after the first MR imaging examination," the authors wrote (Radiology, February 2001, Vol.218:2, pp.562-569).
According to the results, images were successfully acquired in all 19 animals using both agents, and yielded enough data for kinetic analysis. Mean microvascular permeability (Kps) values were significantly higher in carcinomas than in fibroadenomas for both contrast agents, the study stated.
"The overall sensitivity and specificity of Kps for differentiating between benign and malignant tumors with both contrast media was 65% (6 of 14) and 100% (6 of 6), respectively. The positive predictive values were 100%, whereas the negative predictive values were 50% for both macromolecular contrast agents," the authors wrote.
The group concluded that USPIO can successfully characterize tumor microvessels in animals, with USPIO-derived Kps correlating strongly with histopathologic tumor grades.
By Shalmali PalAuntMinnie.com staff writer
February 22, 2001
Related Reading
Contrast agent market to reach $4.22 billion by 2006, July 19, 2000
Click here to post your comments about this story. Please include the headline of the article in your message.
Copyright © 2001 AuntMinnie.com


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











