
Olympic skier Picabo Street knows a thing or two about shattered knees. After winning a silver medal in Lillehammer in 1994, Street crashed in a separate skiing incident and ripped apart her left knee -- just one year and two months before the 1998 Olympic Winter Games in Nagano. But she still managed to take home a gold medal in the Super G competition. Less than a month later, Street suffered another setback at a World Cup race in Switzerland, where she careened into a safety fence and took out her right knee.
Six surgeries, including two anterior cruciate ligament (ACL) reconstructions later, Street hoped the 2002 Olympics would give her a chance to become the first U.S. woman to win three Olympic skiing medals. Alas, the brave athlete's hopes were dashed yesterday when Street finished 16th in her Olympic finale. (France's Carole Montillet turned in a nearly perfect performance to win the women's downhill in 1 minute, 39.56 seconds.)
"This is the last race of my career," Street told NBC on Tuesday. "I’m not going to have to live without skiing. I’m just going to have to live without trying to be perfect on my skis everyday, which is wonderful."
In many cases, when the ACL goes out, the meniscal joint is down for the count as well. The cause of meniscal tears in skiers? Generally, they result from catching the edge of the ski at top speed, resulting in a rotational stress applied to a flexed, weight-bearing knee.
The results of a study on Alpine skiers out of the Aspen Valley Hospital in Aspen, CO, showed that 68% of the ACL injuries in the study’s patient population also involved meniscal tears. Lateral tears were found in 83% of the injured skiers; 17% were medial. Nearly all (98%) of the 317 knees underwent reconstruction within 28 days of injury (American Journal of Sports Medicine, March-April 1995, Vol.23:2, pp.170-172).
But unless we are looking at Picabo Street-caliber injuries, how much, and how often, is follow-up imaging required on these patients? Perhaps less than you think, according to Dr. Thomas Magee, staff radiologist at the Neuro Imaging Institute in Melbourne, FL.
MR arthrography may not be necessary for imaging all postoperative knee patients, said Magee in a presentation at the 2001 RSNA meeting in Chicago.
Patients with meniscal repairs nearly always require MR arthrography to confirm or rule out a re-tear. But subjects with meniscal resections of less than 25% almost always don't need it, according to Magee.
"MR arthrography is necessary in less than 50% of postoperative knee MR examinations," he said.
 |
| MR arthrogram is needed to demonstrate a meniscal tear in a patient with >25% meniscal resection. |
 |
| MR arthrogram demonstrates a meniscal re-tear in a patient with >25% meniscal resection. |
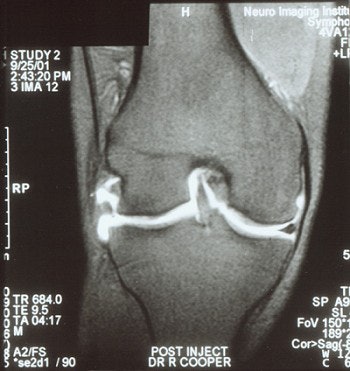 |
| MR arthrogram demonstrates no meniscal tear in a patient with >25% meniscal resection. Images courtesy of Dr. Thomas Magee. |
Researchers from the Neuro Imaging Institute reviewed 100 consecutive postoperative MR knee studies. Of the 100, 78 had preoperative MR exams to review directly in conjunction with the postoperative MR study. All postoperative MR scans were performed within two years of arthroscopy.
Nine of the 100 MR studies indicated avascular necrosis, all 9 of which were documented to be in the area of previous surgery. The researchers found that 19 had marked degenerative joint disease in the area of previous surgery, and 7 had chondral defects or injuries.
Twenty-nine cases had clear evidence of a re-tear without gadolinium injection, while 36 required gadolinium injection to determine whether there was a re-tear, Magee said. The 29 noncontrast cases included findings such as fluid extending into a tear, a tear in a new area, a displaced fragment, or an irregularly truncated meniscus, according to the researchers.
Of the 36 cases requiring contrast, 22 had MR arthrogram evidence that showed re-tear, while 14 had no clear MR finding to explain new or persistent pain post surgery, according to the study team.
The researchers recommended review of a postoperative knee MR without contrast prior to performing MR arthrography. Patients with meniscal resections greater than 25% or with meniscal repair required MR arthrography in the study, however, Magee said.
By Erik L. Ridley
AuntMinnie.com staff writer
February 13, 2002
Copyright © 2002 AuntMinnie.com





















