Children who suffer restless nights from sleep apnea show evidence of a restricted upper airway, particularly where the adenoid and tonsils overlap, according to investigators from the Children’s Hospital of Philadelphia. They used MRI to assess the soft tissues and skeleton that make up the upper airway in 20 children with obstructive sleep apnea syndrome (OSAS), and compared the results with those of 20 control subjects.
"Both anatomic and physiologic factors affecting upper airway size, shape, and function may play a role in the causation of OSAS. Frequently, OSAS is associated with adenotonsillar hyperplasia," wrote Dr. Raanan Arens and colleagues in the American Journal of Respiratory and Critical Care Medicine. However, in children with no apparent adenotonsillar hyperplasia, other abnormalities could be the reason for OSAS, they added (January 1, 2003, Vol.167:1, pp.65-70).
The patients (mean age 3.7 for subjects; 3.9 years for control) were sedated with 2 mg/kg of pentobarbital given intravenously, for a maximum dose of 200 mg. The MR scans were performed on a 1.5-tesla Magnetom Vision system (Siemens Medical Solutions USA, Malvern, PA). An anterior-posterior volume head coil was used for image acquisition, and the patient’s head was positioned supine in the soft tissue Frankfurt plane (tragus of the ear to orbital fissure), as well as perpendicular to the table. Sequential T2-weighted, spin-echo axial sections were acquired from the orbital cavity to the larynx.
The group used a "fuzzy connectedness segmentation" software program that was developed in-house to process the images.
"The MR images…were processed and segmented automatically to compute the airway including its surface description, centerline, and volume," the authors stated. "Fuzzy connectedness is a computational method of object segmentation that takes into account the effects of tissue heterogeneity, imaging noise, and blurring." This program was based on the 3Dviewnix software created by study co-author Jayaram Udupa, Ph.D., at the Medical Imaging Processing Group at the University of Pennsylvania in Philadelphia.
"I read the MRI in all cases after we performed analysis of the data. During the past several years we’ve gained experience with this anatomical region. We have reviewed about 300 MRIs so far of normal children and children with sleep-disordered breathing. Acquisition time was about two minutes in each case," Arens explained in an e-mail to AuntMinnie.com.
Subjects with OSAS underwent polysomnography before the MR exam; control subjects underwent MR of the head for other indications including migraine and concussion. Based on the results of a sleep questionnaire, all control subjects had an apnea score of less than -1, ruling out OSAS as a potential condition.
According to the MR results, the mean cross-sectional area of the total upper airway was 28.1 mm2 in the OSAS group and 47.1 mm2 in the control group. The minimal cross-sectional area of the upper airway was smaller in the OSAS group, 4.6 mm2 versus 15.7 mm2. The upper airway volume was 1,129 mm3 for the children with OSAS and 1,794 mm3 for the control kids.
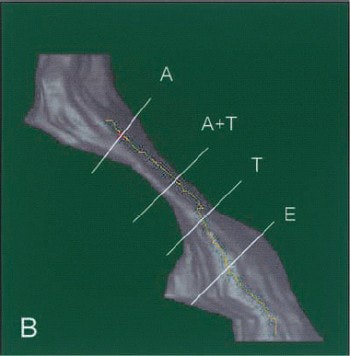 |
| A 3-D display of an upper airway and its centerline in a patient with OSAS. |
"Significantly smaller mean cross-sectional area, minimal cross-sectional area, and volume were noted in subjects with OSAS in the upper 60%-70% of the upper airway," the authors wrote. "Our findings suggest that the upper airway of children with OSAS is restricted along the upper two-thirds of its length and predominantly in the region where the adenoid and tonsils overlap...These observations suggest that flow resistance is higher in these regions, and complete obstruction during inspiration in sleep may be more likely where narrowing occurs and high negative pressures are developed."
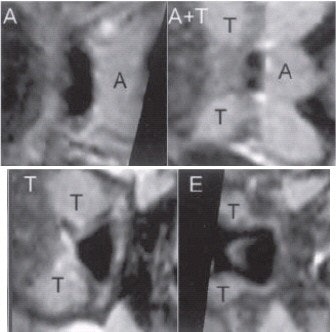 |
| A gray-level, 2-D scene of the cross section of the airway orthogonal to the centerline at marked locations A (adenoid), A and T (adenoid and tonsil overlap), T (tonsils), and E (epiglottis). |
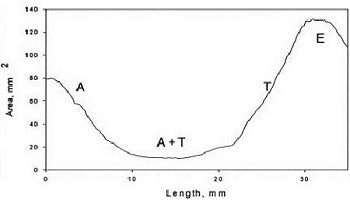 |
| A plot of the cross-sectional area function. Images courtesy of Raanan Arens, Joseph M. McDonough, Aaron M. Corbin, Nathania K. Rubin, Mary Ellen Carroll, Allan I. Pack, Jianguo Liu, and Jayaram K. Udupa, 2003, "Upper Airway Size Analysis by Magnetic Resonance Imaging of Children with Obstructive Sleep Apnea Syndrome," American Journal of Respiratory and Critical Care Medicine, Vol.167, pp.65-70). |
While treatment protocols for OSAS patients are still determined by history, clinical exam, and an overnight sleep study, Arens said his group believes that "in the future MRI may provide a quick and accurate modality for diagnosis of sleep apnea, particularly in cases not resolved by surgery and in more complicated craniofacial syndromes associated with sleep apnea."
In the next phase of research, Arens and colleagues will perform dynamic MR studies, gated to respiration, with the goal of describing the exact location of obstruction during the respiratory cycle in children with OSAS. These images will then be paired with computational flow models to reveal the physiological aspects of the obstructed airways, he added.
A limitation of the current study -- and of pediatric sleep studies with imaging in general -- is the use of sedation, which can reduce upper airway muscle activity and may affect airway measurements. But the alternative to sedation, sleep deprivation, is best done onsite in a sleep lab rather than in an imaging suite, according to researchers from the Children’s Hospital Medical Center in Cincinnati, writing in an earlier paper.
This group tested their institution’s structured sedation program during dynamic sleep fluoroscopy of children with OSAS. In their study of 80 exams, 90% of the studies were successfully performed with conscious sedation; four patients required sedation by an anesthesiologist. he remaining 10% fell asleep without sedation. The specific cause of sleep apnea was determined in 83% of the children. None of the children suffered any complications.
"The goal of sedation...is to reproduce the conditions of sleep that often lead to some degree of airway compromise," wrote Dr. Lane Donnelley and colleagues.
"Although the potential of airway compromise should be considered in patients being evaluation for sedation, a history of obstructive sleep apnea in itself is not a contraindication for conscious sedation" (American Journal of Roentgenology, November 2001, Vol.177:5, pp.1031-1034).
By Shalmali PalAuntMinnie.com staff writer
January 24, 2003
Related Reading
Pediatric sedation risk lowered when guided risk assessment performed, February 6, 2002
Melatonin puts kids to sleep, makes MRI a dream, December 10, 2001
MRI could be dream modality for pediatric sleep-related breathing problems, May 22, 2001
Tracking of pediatric sedation for MR imaging highlights concerns, July 11, 2000
Copyright © 2003 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)