
How useful is low-field MR in assessing musculoskeletal issues? A series of recent studies has tackled this question. The known benefits of low-field MR include greater comfort for claustrophobic and obese patients, a lower purchase price, and easier maintenance.
However, in terms of image quality, low-field MR has its drawbacks, such as longer imaging time, lack of fat suppression, and greater image noise, according to a group from Florida. They found that low-field MR did not prove terribly useful for pinpointing small tendon tears of the shoulder.
Nevertheless, low-field MR does offer some advantages over high-field MR in certain orthopedic imaging circumstances. A Dutch group found it had value in patients with knee trauma, while researchers from Japan said that low-field MR could offer unique information on periprosthetic tissue after failed hip arthroplasty.
Low-field MR of the shoulder
While studies have compared low-field and high-field MR interpretations before, they have done so either retrospectively or by using two different groups of patients. Dr. Thomas Magee and colleagues from the Neuroimaging Institute in Melbourne, FL, went a step further in their prospective evaluation of the modality with a single patient cohort.
"We undertook this study to determine whether imaging the same patients on both high (1.5-tesla) and low-field-strength (0.2-tesla) units would affect MRI interpretations, and if so, whether these differences in interpretation would affect clinical treatment," they wrote (American Journal of Roentgenology, November 2003, Vol. 181:5, pp. 1211-1215).
The study population consisted of 40 patients who agreed to undergo complete shoulder MR exams on an open system and a high-field system (both from GE Medical Systems, Waukesha, WI). The MRI sequences on the low-field system included coronal T1-weighted images, T2-weighted images, and STIR images. On the 1.5-tesla scanner, coronal and sagittal fast spin-echo T2-weighted images were obtained. A phased-array shoulder coil was used in all cases.
For the prospective review, one musculoskeletal radiologist analyzed both sets of images for the presence or absence of supraspinatus tendon tears, superior labral anteroposterior tears (SLAP), and anterior or posterior labral tears. All 40 exams were then retrospectively reinterpreted by consensus of three radiologists.
According to the results, the high-field MR images altered the reviewers’ interpretations of low-field MR images for nine of 40 cases. In four patients, the open MR did not show full-thickness suprasinatus tendon tears, all of which were seen on the high-field MR results. Also, three labral tears and two superior labral anteroposterior lesions could not be depicted on the low-field exam, but were seen on the high-field images.
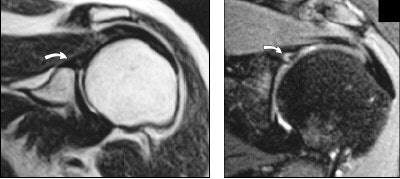 |
| Thirty-eight-year-old women with shoulder pain. Left, T2-weighted coronal 0.2-tesla image (TR/TE, 3,350/94.5) shows suspected abnormality in superior labrum (arrow). STIR coronal imaging was attempted, but patient could not remain motionless long enough. Right, T2-weighted coronal 1.5-tesla image (2,500/68) shows definite superior labral anteroposterior tear (arrow) that was confirmed at arthroscopy. Magee, T, Shapiro, M, Williams D, "Comparison of High-Field-Strength Versus Low-Field-Strength MRI of the Shoulder," (AJR 2003, Vol.181, pp.1211-1215). |
Magee and co-authors concluded that 1.5-tesla MR imaging was inherently superior to low-field MRI, offering better signal-to-noise ratio (SNR), faster imaging, and thinner slices.
"This most likely resulted in better visualization of subtle signal abnormalities...these small tears did not resolve as well on the low-field-strength units because the larger slice thickness needed to maintain adequate SNR required more volume averaging," they wrote.
Peripheral joint injuries
In a poster presentation at the 2003 RSNA conference, investigators from the Netherlands used low-field dedicated extremity MR to evaluate all patients with trauma of the wrist, knee, or ankle.
"The initial diagnostic strategy for the management of acute wrist, knee, and ankle injury generally consists of patient history, physical exam, and, if a fracture is suspected, conventional radiography," wrote Dr. Jeroen Nikken and colleagues from Erasmus University Medical Center in Rotterdam. "This strategy is adequate to detect fractures; however, it is not very accurate in detecting soft-tissue injuries."
While MR may be the preferred imaging modality for these types of injuries, its high cost and limited availability are two stumbling blocks. "However, the use of a short examination protocol on a relatively inexpensive low-field dedicated extremity MRI system may prove to be feasible," the authors suggested.
For this study, 500 patients with recent trauma of the wrist, knee, or ankle were randomized between x-ray (labeled the reference group) and a combination of x-ray and low-field MR (called the intervention group). Symptoms included pain and swelling, and the patients presented within seven days of onset. The MR imaging was done on an Artoscan M (Esaote, Genoa, Italy).
The outcome measures were quality of life, time to completion of diagnostic work-up, number of additional diagnostic procedures after the initial hospital visit, and convalescence time. A cost analysis was done as well. Quality of life was measured with the EuroQol and SF-36 (standardized instruments for measuring healthcare outcomes) survey questionnaires at four points in time, up to six months after the injury.
For wrist injuries, the reference group required six additional diagnostic procedures; were absent from work for five weeks; and the convalescence time was 54.3 days. For the intervention group, the number of additional diagnostic procedures was three; they were absent from work for 8.6 weeks; and convalescence time was 49.6 days.
For knee injuries, the reference group had 9 additional diagnostic procedures; stayed out of work for 12.4 days; and required 76.6 convalescent days. Those that had an MR also had 3.5 extra procedures; were absent from work for 9.6 days; and needed 66.2 convalescent days.
Finally, for the ankle injuries, the reference group need one additional procedure; missed 12.6 days on the job; and needed 55.9 days for convalescence. For the intervention group, one additional procedure was done; 11.2 days of work were missed; and the convalescence time was 54 days.
"In the knee-injured patients, the EuroQol tariff was significantly higher in the intervention group, one week and six weeks after the initial trauma, and the SF-36 physical functioning score was significantly higher at one week," the authors stated. "Although for all joints the time to convalescence was shorter in the intervention group, the differences were not significant."
In terms of cost, only the patients with knee injuries saw a benefit with the addition of MR -- 1,820 euros for the intervention group versus 2,231 euros for the reference group.
They concluded that a low-field MR exam did not significantly impact the course of treatment for wrist and ankle injuries. But for patients with knee injuries, adding MRI "shortens the time to completion of diagnostic work-up, reduces the total number of additional diagnostic procedures, and improves the quality of life in the first six weeks."
Failed hip arthroplasty
Dr. Hideuhaur Sugimoto and co-authors used 0.5-tesla MR imaging to investigate the relationship between periprosthetic signal intensity and x-ray, surgical, and pathologic findings. They conducted their study at Showa University Fujigaoka Hospital in Kanagawa, Japan.
"Revision of the (total hip arthroplasty) prosthesis is still required when loosening occurs," they wrote. "Loosening of the prosthesis is generally diagnosed on the basis of radiographic demarcation of the prosthetic component, either by a progressive widening of the radiolucency at the bone-cement and/or the cement-stem interface, or by a change in position" (Radiology, December 2003, Vol. 229:3, pp. 718-723).
However, these findings are not always indicative of loosening, which a low-field MR exam might be better at determining, they explained.
For this study, 22 consecutive female patients who had undergone revision surgery for failed hip arthroplasty were included. Revision was required for a number of reasons, including loosening of the femoral component, breakage, and infection.
All underwent MR, prior to surgery, on a 0.5-tesla system (Contour, GE Medical Systems, Waukesha, WI) with a flexible quadrature coil wrapped around the pelvic girdle. Oblique coronal images were obtained and the MR protocol included STIR, spine-echo, and T1-weighted images. For MR image analysis, the periprosthetic region was divided into seven femoral Gruen zones and further subdivided for a total of 157 zones (Clinical Orthopaedics, June 1979, Vol. 141, pp. 17-27).
Two observers retrospectively analyzed the signal intensity patterns on imaging, comparing them with surgical and pathological results. The authors concluded that the overall MR signal intensity patterns fell into three types: either greater than (type 1), equal to (type II), or less than bone marrow (type III) on the images, with or without contrast.
They found that periprosthetic MR signal intensity was a type I in the distal femur on the fast STIR images with no contrast enhancement on T1-weighted images in 11 zones. And they reported that signal intensity was type I on fast STIR images with contrast enhancement in 45 zones. Finally, the signal intensity was type III on the fast STIR images with no contrast enhancement seen.
Compared with radiography, the MR depicted a type III pattern in zones where the x-ray showed normal bone tissue and a stable stem, the authors reported. MR signal intensities also correlated well with pathologic and surgical findings.
Overall, the group praised low-field MR for yielding pertinent information, especially for the preoperative assessment of stem loosening. In addition, "there was a significant association between the total number of specific MR signal intensity patterns and stability of the femoral prosthesis," they wrote.
By Shalmali PalAuntMinnie.com staff writer
December 22, 2003
Related Reading
MRI, US make sense of disorganized scar tissue in PTTL injuries, October 29, 2003
MR findings predict short-term pain relief after intra-articular injection, October 20, 2003
Just (over) Do It! Imaging pegs overuse injuries in specialty sports, October 8, 2003
MR categorizes acute hamstring injuries for pre-op assessment, September 29, 2003
MR arthrography not always needed in post-operative knees, February 13, 2002
Copyright © 2003 AuntMinnie.com




















