Cardiac imaging sessions at the 2003 RSNA meeting in Chicago featured three papers on the role of dobutamine stress MRI, as well as contrast-enhanced MRI, in assessing the myocardium. Two groups, from the Netherlands and Germany, discussed the safety and feasibility of dobutamine MR in patients suspected of having myocardial ischemia.
In a separate paper, the same German investigators also shared their experienced with contrast-enhanced MR and dobutamine stress echocardiography for determining myocardial viability.
Myocardial ischemia
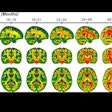
The patient population for the first study consisted of 400 consecutive patients with suspected myocardial ischemia. Specifically, dobutamine cardiac MR was used to identify wall motion abnormalities of the left ventricle, which can be indicative of ischemia, explained presenter Dr. Caroline Janssen from the University Hospital in Groningen, the Netherlands.
The patients, 49% of who had known coronary artery disease, underwent imaging on a 1-tesla MR unit with ECG-gating (Harmony, Siemens Medical Solutions, Erlangen, Germany). Cine short axis cardiac MR images of the left ventricle were acquired at rest and during a standardized high dose tagged dobutamine cardiac MR protocol. Dobutamine was infused at doses of 10, 20, 30, and 40 μg/kg/min. for six minutes per level.
According to the results, dobutamine cardiac MR exams were successful in 95% of the patients. The exam time was 48 minutes. Thirty one percent (112) showed new wall motion of abnormalities, which was indicative of myocardial ischemia.
Although there were no myocardial infarctions or fatal complications brought on by the exam, 9.5% of the patients (38) did have unreadable exams because of side effects including breath artifacts, claustrophobia, or because of their anti-anginal medicine.
"Most of the patients stopped their medication four days before the study, however there were a few who (did not)," Janssen told AuntMinnie.com. "It is difficult to avoid this problem."
 |
| Two midventricular images at 10 and 40 μg/kg/min. of dobutamine. The arrow (at 40 μg) indicates absence of septal wall thickening, which is indicative of inducible myocardial ischemia. Image courtesy of Dr. Caroline Janssen. |
The exam had to be terminated in three patients because of cardiac arrhythmias. Other minor complications included symptomatic and severe hypotension, nausea, and vomiting. Only patient suffered ventricular fibrillation, which was successfully treated with resuscitation, Janssen reported.
The group concluded that dobutamine cardiac MR is a safe and feasible test in patients with suspected myocardial ischemia. Janssen added that doing the exams did not prove to be too taxing to the MR suite schedule as the group allotted one morning a week to dobutamine cardiac MR exams, imaging 3-4 patients consecutively.
Dobutamine CMR has been performed routinely at her hospital since 1999, Janssen said. Dr. Dirkjan Kuijpers and colleagues outlined the department’s imaging protocol in the April 1, 2003 issue of Circulation (Vol.107:12, pp.1592-1597).
A second study from the University of Essen in Germany also found dobutamine MR studies to be a safe and accurate diagnostic test in patients.
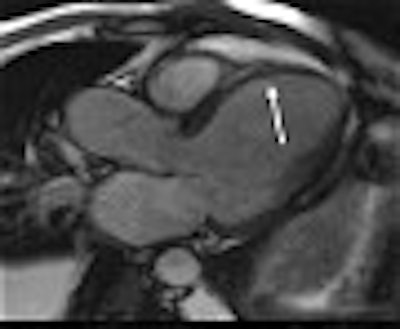
This study group consisted of 329 patients with suspected or known coronary artery disease. In the latter case, the patients had been referred for high-dose stress dobutamine MR assessment of hemodynamic significance of stenoses, said presenter Dr. Jörg Barkhausen.
All exams were performed on a 1.5-tesla Magnetom Sonata (Siemens Medical Solutions, Erlangen Germany). A dobutamine/atropin stress protocol was used until 85% of the age-predicted heart rate was achieved. The infusion rate was 10, 20, 30, and 40 μg/kg/min of dobutamine and up to 1 mg of atropin. The exams took about 40 minutes.
At least three long- and three short-axis views were obtained at each stress level, using a steady state, free precession sequence (TR 3 ms, TE 1.5 ms, FA 60° ), the authors stated in their abstract.
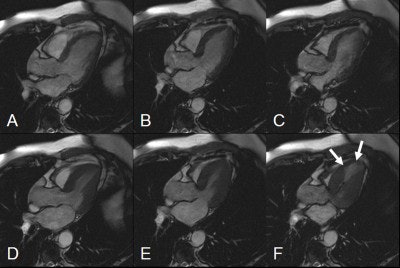 |
| Diastolic (A-C) and systolic (D-F) images in the left ventricular outflow tract view. Images at rest (A and D) and low-dose (B and E) show normal contractility. At high-dose dobutamine (C and F), a stress-induced wall motion abnormality (arrows) can be detected. Image courtesy of Dr. Jörg Barkhausen. |
An experience radiologist and cardiologist came to a consensus agreement when evaluating the exams. Myocardial ischemia was defined by new or worsening wall motion abnormalities in more than one myocardial segment.
According to the results, dobutamine stress MR yielded a sensitivity of 81.8%, a specificity of 91.7%, an 81.5% negative predictive value, and a 91.8% positive predictive value in patients with coronary artery stenosis (luminal narrowing > 75%). These results were confirmed with coronary angiography in 103 patients within 14 days of dobutamine stress MRI.
Clinical follow-up was done on 215 patients without stress-induced wall motion abnormalities, Barkhausen said, and at the time of his RSNA presentation, there were no reports of cardiac events.
The complication rate in this study was 5% (16/318 patients), and included sustained ventricular tachycardia, atrial fibrillation, and nausea. In 3.4% of the patients, dobutamine stress MRI could not be performed because of claustrophobia as well as non-diagnostic imaging quality due to arrhythmia.
His group plans to follow these patients for the next five years, Barkhausen told AuntMinnie.com.
Myocardial viability
When it comes to surveying myocardial viability, Dr. Peter Hunold, Barkhausen, and colleagues found that contrast-enhanced MRI fared better than dobutamine stress echocardiography (DSE). They looked specifically at late enhancement on MR in patients with CAD and impaired left ventricular (LV) function.
"We do use MRI (routinely at our institution) for viability assessment because it seems to be better than the reference standard PET. DSE is not very accurate," Hunold told AuntMinnie.com in an email.
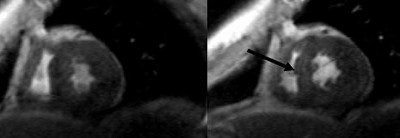
The patient population consisted of 19 patients with proven CAD and impaired LV (32% ejection fraction). Both imaging exams were done before coronary artery bypass grafting (CABG) surgery. The MRI was done on a 1.5-tesla Magnetom Sonata unit and consisted of a cine study in long and contiguous short axis orientations of the LV. A TrueFISP sequence was used.
Finally, short axes were scanned with a segmented inversion-recovery TurboFLASH sequence, 8-15 minutes after the administration of 0.2 mmol/kg of Magnevist (Schering AG, Berlin). The latter sequence was done for detecting late enhancement, which was classified on a four-point scale, with a score of 1 equaling no late enhancement and a score of four indicating transmural late enhancement.
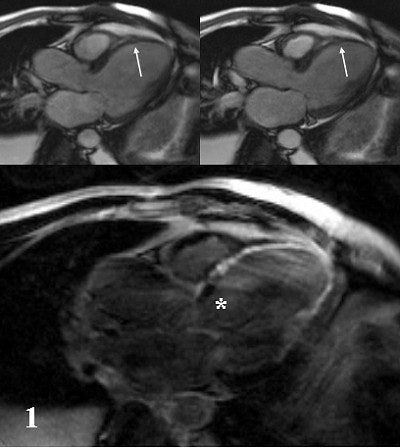 |
| A 42-year-old male patient after large myocardial infarction. Top, diastolic (left) and systolic (right) TrueFISP Cine images in LVOT orientation. Arrows show a large akinetic area in the anteroseptal wall. Bottom, IR-TurboFLASH image done 10 minutes after administration of gadolinium. The bright area shows transmural infarction (late enhancement) of the anteroseptal, apical and inferolateral wall. Asterisk shows a small akinetic area without late enhancement in the basal anteroseptal wall. |
DSE was performed at rest, and under stress, during the infusion of 5 and 10 μg/kg/min of dobutamine. "The regional wall motion was judged as normal, hypokinetic with recruitment under stress indicating myocardial hibernation," the group wrote in their abstract. Hypokinetic wall motion without change under stress was labeled as scarring.
In total, 323 myocardial segments were analyzed. On MRI, 168 segments (52%) had a score of 1, while 44 segments (14%) showed transmural late enhancement (score 4). Non-transmural scars were detected in the remaining segments.
On DSE, 133 segments (41%) had normal wall motion and 33 (10%) showed hypokinetic segments that improved at stress (hibernation). Of these 133 segments, late enhancement occurred 35% (46). Of the 33 segments, 88% had MRI scores of 1 or 2 (subendocardial late enhancement of <50% of wall thickness).
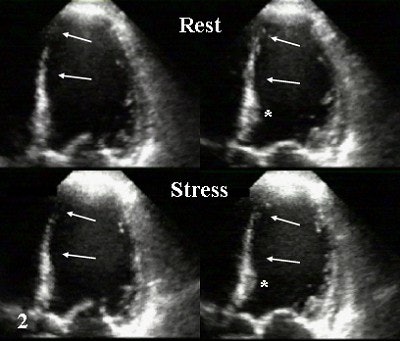 |
| The same patient. Echocardiography in corresponding apical LVOT view. Top, diastolic (left) and systolic (right) image in rest study. Bottom, diastolic (left) and systolic (right) image during infusion of 10 µg/kg/min. of dobutamine (Stress). Arrows show akinesis in rest and under stress indicating scar corresponding to MRI. Asterisk shows slight improvement of basal segment under stress, indicating viable but ischemic myocardium as suggested on MRI. Images courtesy of Dr. Peter Hunold. |
Forty-nine percent of the hypokinetic segments (157) did not change at stress and were classified as scar tissue by DSE. Of these 157 segments, 61% showed late enhancement.
Finally, of the 91 segments with a late enhancement score of 3 or 4, DSE characterized only 77% (70) as not viable. These segments were not expected to improve function after revascularization, Hunold said.
The group concluded that, in comparison to contrast-enhanced MRI, DSE had a tendency to overestimate scar tissue in these patients. Thus, MRI offered a more robust measurement of myocardial viability, Hunold said.
However, Hunold did offer one caveat: In about one-third of segments without evidence of scar on MRI (no late enhancement), DSE did not reveal improvement under stress. This may contribute to the number of segments that don’t improve after revascularization.
"We do not yet know the reason for that," Hunold explained. "But this very well matches some other data of ours which shows that, after revascularization, some segments do not improve although sufficiently operated (on). So, from those older data we know that the lack of late enhancement really does not necessarily mean that revascularization will be successful. Our idea is that the non-improving DSE segments might be those with no improvement after revascularization."
By Shalmali PalAuntMinnie.com staff writer
February 6, 2004
Related Reading
Dobutamine echo best for assessing cardiac risk with major vascular surgery, November 14, 2003
Subtle LV dysfunction seen with early diabetic heart disease, August 13, 2003
PET may overpredict myocardial recovery compared with MRI, March 11, 2003
Copyright © 2004 AuntMinnie.com


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)