The three little letters "TMJ" seem wholly inadequate to describe disorders of the temporomandibular joint. The grab bag of symptoms include facial pain, jaw pain, earache, lockjaw, headache, misaligned bite, neck and shoulder pain, swelling, and jaw clicking.
Some possible causes of TMJ are arthritis, displacement of the disk that is located between the jawbone and socket, rheumatoid arthritis, and trauma. Teeth grinding, especially during sleep, can be another culprit.
And the treatment options are no less broad, ranging from conservative dental care (mouth guards, muscle relaxants) to more complex, invasive surgical procedures. In a worst-case scenario, surgery for other reasons, such as bilateral sagittal split osteotomy (BSSO), can cause changes in the TMJ disk.
In the face of so much uncertainty, imaging plays an important role in TMJ management. Recent European studies indicate that MRI may be a clinically useful way to study the articular disk and the joint as a whole. Additionally, oral surgeons from the University of Washington in Seattle turned to MRI to evaluate TMJ disk position in patients who had undergone BSSO with rigid fixation. However, the high cost of MRI does make it slightly less advantageous than other modalities, according to a third report.
AD and disk displacement
Investigators from J.W. Goethe University in Frankfurt-Main, Germany, looked at whether dynamic MRI was feasible for visualizing the articular disk (AD) in near real-time.
The patient population consisted of 17 patients, with five TMJ patients and a dozen healthy subjects. All underwent sagittal near-real-time imaging (NRTI) of the TMJs, using a true-FISP sequence on a 1.5-tesla scanner. Two observers then rated AD depiction on a scale of 1 to 4, with 1 indicating very good results.
The study showed that disk motion, including fast reposition movements, was clearly depicted in patients with internal derangement. Image quality scored low at 2.4, however, due to degenerative changes of the AD. The ADs of the control group were visualized with high quality in all stages of movement (1.69).
"According to the preliminary results of this feasibility study, the suggested NRTI true-FISP sequence is capable of visualizing the entire motion of the AD of the TMJ in normal and pathologic stages with high quality. Further studies are needed to prove the clinical usefulness of this new technique," they wrote (European Radiology, October 2004, Vol. 14:10, pp. 1889-1894).
In an earlier, separate paper, Dr. Oliver Sommer and colleagues declared that MR is the "modality of choice in presumed internal derangement and inflammatory arthritis, and allows the clinician to apply therapeutic strategies optimally suited to the underlying abnormality" (RadioGraphics, August 14, 2003). The group is from Hospital Lainz in Vienna, Austria, and the University of Innsbruck, also located in Austria.
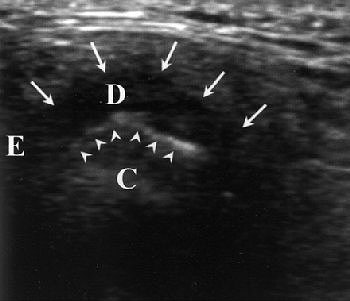 |
| Temporomandibular joint (TMJ) of 32-year-old woman. Diagnosis of disk displacement with reduction was based on MR imaging findings. Longitudinal high-resolution sonogram obtained in closed-mouth position shows anterosuperior TMJ compartment and disk (arrows) anterior to condyle (arrowheads). E = articular eminence, D = disk, C = condyle. Emshoff R, Jank S, Bertram S, Rudisch A, Bodner G, "Disk Displacement of the Temporomandibular Joint: Sonography Versus MRI," (AJR 2002; 178: 1557-1562). |
The modality's strengths include superior tissue contrast and high-resolution imaging with surface coils for depicting TMJ anatomy and abnormalities. Additionally, concurrent imaging of the closed and open jaw allows for functional and morphologic assessment, as well as proper grading of AD disease processes, they wrote.
Their standard MRI protocol for TMJ was as follows:
- Circular polarized transmit-receive TMJ coil
- Sagittal and coronal proton density-weighted (PDW) sequences, closed and open jaw
- Sagittal and coronal STIR sequence, closed jaw
- No contrast
The group said that the STIR sequences were a cost-effective alternative to fat-saturated contrast material-enhanced T1-weighted sequences.
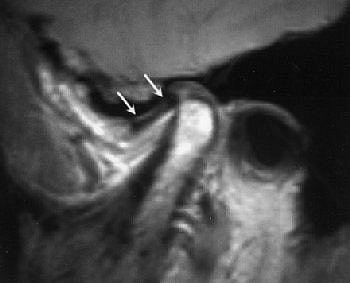 |
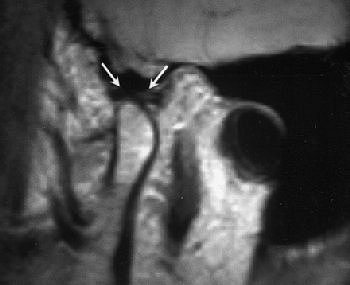
Same patient. Above, sagittal MR image obtained in closed-mouth position shows anterosuperior TMJ compartment and disk (arrows) anterior to condyle. Below, sagittal MR image obtained in maximal open-mouth position shows anterosuperior TMJ compartment and disk (arrows) superior to condyle. Emshoff R, Jank S, Bertram S, Rudisch A, Bodner G, "Disk Displacement of the Temporomandibular Joint: Sonography Versus MRI," (AJR 2002; 178: 1557-1562).
 |
The high price tag for MRI was one reason that two of Sommer's co-authors did a comparison study between the modality and ultrasound for disk displacement of TMJ.
In the second study led by Dr. Rudiger Emshoff, 64 consecutive patients at the University of Innsbruck underwent MR scans on a 1.5-tesla scanner, using the protocol described above. They also had sonographic scans using a 12-MHz linear-array transducer.
MR revealed 87 cases of internal derangement, of which 22 were true-positive (TP) findings of disk displacement with reduction (82% sensitivity) and 50 were TP findings of disk displacement without reduction (95% sensitivity). There were 15 instances of false-positive (FP) results, the majority of which wrongly indicated displacement without reduction.
In comparison, ultrasound detected 81 instances of internal derangement (95% accuracy), 22 cases of disk displacement with reduction (92% accuracy), and 50 instances of disk displacement without reduction (90% accuracy). There was one FP finding for internal derangement. Most of the disk displacements missed on sonography were positioned laterally or medially, the group wrote.
"While MR imaging has a diagnostic accuracy of 95% when coronal and sagittal imaging techniques are combined ... MR imaging poses a problem in terms of clinical availability and cost," the authors wrote. "Sonography, despite its limitations, may provide valuable information" (American Journal of Roentgenology, June 2002, Vol. 178:6, pp. 1557-1562).
However, the researchers noted that MRI should continue to serve as the gold standard in future comparative imaging studies of TMJ.
TMJ after mandibular advancement
Bilateral sagittal split osteotomy (BSSO) with rigid fixation is commonly used to treat mandibular retrognathia (underdeveloped lower jaw). But TMJ symptoms don’t always resolve after orthognathic surgery, according to a presentation at the American Association of Oral and Maxillofacial Surgeons (AAOMS) meeting earlier this month.
"There's a great deal of controversy regarding patients with preoperative AD displacement, and pre-existing TMJ, who undergo orthognathic surgery," explained Dr. Jessica Lee from the University of Seattle in Washington.
"What do we tell these patients? They are about to embark on surgical treatment. Do we tell them: 'The surgery that you are just about to have is going to improve your TMJ or worsen it'?" added Lee, who is the residency program director at the university's department of oral and maxillofacial surgery.
The goal of this study was to examine TMJ disk position in symptomatic patients before and after BSSO advancement, and to determine whether disk position on MRI correlated with changes in clinical symptoms.
 |
Fifty-year-old woman with clicking and pain in both TMJs, 8-mm mandibular advancement, and MIO that decreased from 42 mm to 40 mm postoperative. Above, bilateral, right anterior disk displacement on MRI preoperative, which did not change on postoperative MRI, below. Images courtesy of Dr. Jessica Lee.
 |
The study population consisted of 30 temporomandibular joints in 15 patients with preoperative pain and clicking. All patients underwent BSSO with rigid fixation between 1999 and 2001 for class II mandibular retrognathia.
They underwent preoperative and post-treatment scans on a 0.5-tesla scanner. In an e-mail to AuntMinnie.com, Lee shared her group's MRI protocol:
"Proton density images with the following parameters were used: TR 2400, TE 31 msec, NEX 2, field of view 12 cm, slice thickness 2.2 mm with a skip of 0.3 mm, and a matrix (of) 512 x 256. Views were performed both in normal occlusion and with mouth opening of 35 mm. To depict both the condyle and the anterior displaced disk in the same image, a new plane for the coronal imaging was used. Instead of the axial localizer to set up the coronal imaging, the sagittal/oblique closed-mouth images were used. The imaging plane was oriented perpendicular to the posterior slope of the articular eminence and the disk. Seven 2.2-mm slices were obtained with a skip of 0.3 mm covering the whole joint (TR 1500, TE 31)," she wrote.
A maxillofacial radiologist, blinded to the chronological sequence of the MR studies, read the scans. The radiologist looked at the disk position in closed- and open-mouth views, as well as coronal views. The Oswald criteria were used to determine if the AD was normal. A normal AD would be one where the intermediate zone of the disk is located between the condyle and the articular eminence, Lee said.
Based on the preoperative MRI results, 66.7% of the joints had anterior disk displacement with reduction, and 13.3% showed anterior disk displacement without reduction. Six joints had positions that were called intermediate.
Postoperatively, the anterior disk position remained unchanged in 73.3% of the cases, while 16.6% indicated slight medial or lateral displacement of the anterior disk on coronal MR images. Only one joint showed slight improvement in anteroposterior disk position after surgery.
 |
Same patient. Postop lateral displacement of right disk. Pain improved in both joints; clicking resolved in left joint only. Images courtesy of Dr. Jessica Lee.
 |
However, these changes in AD position did not correlate with patient symptoms. Prior to surgery, 70% of the joints had clinically detectable clicking. This was reduced to 11% postsurgery. Pain was noted in 80% of the cases before BSSO, which reduced to 13% after treatment. The mean maximal incisor opening (MIO) was 43.8 mm before treatment and 41.6 mm afterward.
In the majority of patients, TMJ symptoms improved, Lee reported. In two cases, symptoms did not improve, but the patients said their pain intensity did not increase either. Three months postprocedure, there was no further alteration in disk morphology or bony contour of the condyle.
"BSSO advancement with rigid fixation did not result in major alteration of TMJ disk position in our series," Lee concluded. "The overall TMJ symptoms did improve, regardless of the disk position observed on MRI."
Lee said that MRI is reserved for orthognathic surgical patients with more severe TMJ symptoms in order to document their baseline TMJ status, particularly if they will require more TMJ-related treatment in the future.
"(CT scans) are another alternative to assess joint status, although it gives limited information if there is a more severe problem with disk such as perforation," she added.
Lee said that her group plans to continue with this research with a larger patient population and compare the results to a control group.
By Shalmali Pal
AuntMinnie.com staff writer
October 15, 2004
Related Reading
Nailed in the head: X-ray, CT show patient's good luck, July 13, 2004
Sonography has a lock on TMJ, July 22, 2002
Copyright © 2004 AuntMinnie.com