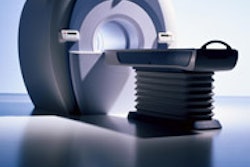
While the use of breast MR is rapidly growing, it's still not a viable replacement for breast biopsy, according to a study in the latest issue of the Journal of the American Medical Association. Low specificity remains the modality's main stumbling block in this setting.
"Use of (breast MRI) for Medicare patients increased almost 3-fold between 2001 (3,440 examinations) and 2003 (10,115 examinations)," wrote Dr. David Bluemke, Ph.D., and colleagues. But "the optimal imaging method (3-dimensional MRI or dynamic MRI) remains controversial" and "the negative predictive value is not sufficiently high ... to use MRI as an alternative to ... breast biopsy for suspicious lesions" (JAMA, December 8, 2004, Vol. 292:22, pp. 2735-2742).
Bluemke and his 16 co-authors are part of the International Breast MRI Consortium (IBMC) study, which includes data from 14 institutions in the U.S., Canada, and Germany.
For this study, 891 women were enrolled, the majority of whom (84.7%) had an abnormal mammogram. In this group, there were 404 malignant index lesions, 341 of which were invasive carcinoma.
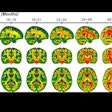
All patients underwent high-resolution, gadolinium-enhanced, T2-weighted 3D MRI. Characteristics of malignant, enhancing lesions on 3D MR included a focal mass with irregular or speculated margins, ductal distribution, or rim enhancement.
Those with enhancing abnormalities were asked to return 18 hours later for a dynamic MRI exam with additional contrast. T1-weighted 2D images centered on the focal abnormality were acquired. Lesion enhancement on dynamic MRI was reader-classified as washout, plateau, delayed, or indeterminate.
According to the mammographic findings, 59.8% of the lesions were BI-RADS 4 and 24.8% were category 5. Of these 695 patients, 367 had ductal carcinoma in situ (DCIS) or invasive cancer, yielding a positive predictive value (PPV) of 52.8% for the modality.
On 3D MRI, 356 out of 404 malignant cancers were identified (DCIS or invasive) as malignant for a sensitivity of 88.1%. MRI was negative for malignancy in 281 cases for a specificity of 67.4%. The PPV for MRI was 72.4%, and the negative predictive value (NPV) was 85.4%, according to the authors. For cases of DCIS, MRI's sensitivity was 73%; for invasive cancer, it was 90.9%.
In all patients, the sensitivity of dynamic MRI alone was 20.5% (with washout curve), and the specificity was 90.4% (no washout curve). "Using either plateau or washout curve as an indicator of malignancy yielded a sensitivity of 63.2% and a specificity of 65.4%," the group stated.
Finally, the area under the receiver operating curve (AUC) for MRI pooled over all institutions was 0.88 (95% confidence interval, 0.86-0.91). While MRI performance was not significantly affected by mammographic breast density, tumor histology, or menopausal status, its sensitivity was greatest in patients with fatty breasts, they wrote.
"Our results indicate that the specificity of MRI is only moderate (67.4%)," the authors stated. While adding dynamic MRI to 3D MRI has the potential, in some situations, to improve specificity, its lackluster NPV does not make it a suitable substitute for tissue sampling.
In an accompanying editorial, Dr. Monica Morrow from the Fox Chase Cancer Center in Philadelphia stated that the study did not justify the routine use of MR.
"In this study, significant numbers of invasive cancers of all sizes were not detected by MRI.... As in other studies, the sensitivity of MRI for the detection of intraductal carcinoma was significantly lower than for the detection of invasive carcinoma," she stated (JAMA, December 8, 2004, Vol. 292:22, pp. 2779-2780).
Despite these less-than-ideal results, Morrow speculated that MRI use has increased over the years because of a perception that the modality improves patient selection for breast-conserving therapy.
But she cautioned that MRI's high sensitivity was not enough to make it an indispensable part of preoperative evaluation. Some of the questions that still need to be answered are whether MRI results can reduce the rate of ipsilateral breast recurrence or identify cancer patients who don't require irradiation.
Bluemke's group acknowledged that more multicenter trials are required to develop true estimates of breast MR's performance. In MR's favor, they pointed out that it does have a role in women with dense breasts as it is only mildly affected by tissue density. Other research has also validated MRI's superiority over mammography in women with a genetic risk for breast cancer.
By Shalmali Pal
AuntMinnie.com staff writer
December 7, 2004
Related Reading
MRI finds breast cancers missed by mammography in high-risk women, December 2, 2004
MRI best for women with heredity risk of breast cancer, September 14, 2004
Copyright © 2004 AuntMinnie.com


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)