Three-dimensional contrast-enhanced MR angiography (3D CE-MRA) is the way to go for diagnosing and treating aortic dissection, according to a group from Changhai Hospital in Shanghai, China. The advantages of 3D CE-MRA in this setting are its speed, efficacy, and noninvasiveness.
"The key to saving lives in aortic dissection is timely diagnosis," said Qi Liu, Ph.D., in a presentation at the 2004 RSNA meeting in Chicago. More specifically, a goal is to determine the right time for elective surgery -- when the operative risk is lower than the risk of dilation-related complications -- and decrease the call for urgent surgical procedures (Italian Heart Journal, September 2004, Vol. 5:9, pp. 648-655).
For this study, 136 patients with aortic dissection underwent MRA after an injection of 0.2 mmol/kg of gadolinium. Of the 136 patients, 21 had surgery, 32 had digital subtraction angiography, and the reminder underwent two exams with ultrasound, CT, MRI, or CT angiography. For the MRA scan, a 3D-FISP sequence was used. The acquisition time was 20 seconds after contrast injection. The source images were subsequently postprocessed using volume rendering (VR), maximum intensity projection (MIP), virtual endoscopy (VE), and multiplanar reformation (MPR).
The results showed that double lumen and intimal flap was evident in all 136 patients. There were 107 DeBakey type III dissections, 27 type I dissections, and two type II dissections. Three-dimensional contrast MRA achieved a diagnostic accuracy of 100%, and classified the diagnosis in 99% of the cases.
 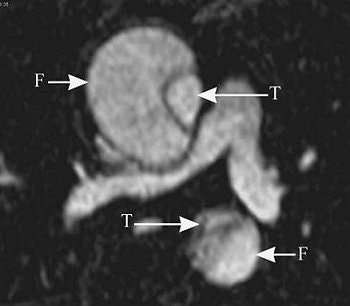 |
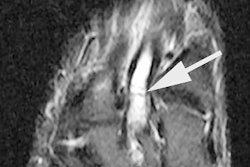
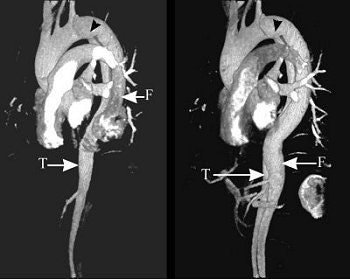
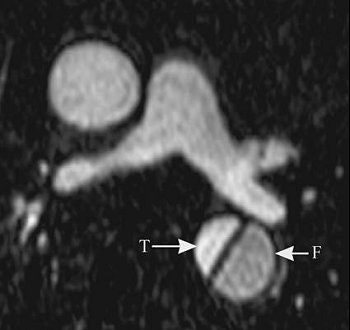
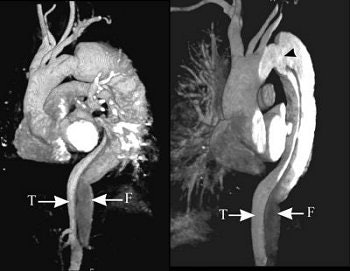
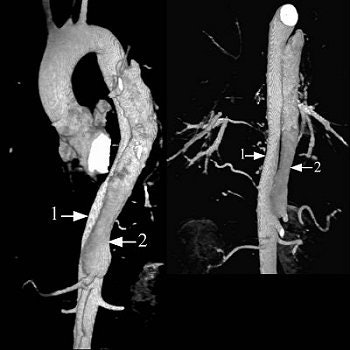
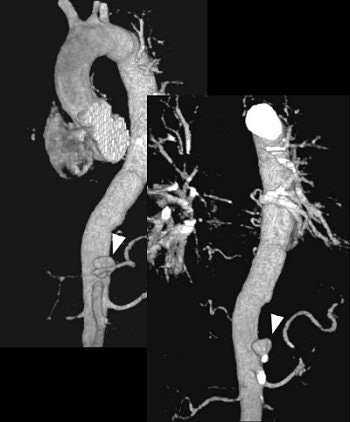
The series of images illustrate the typical manifestations of aortic dissection, including Stanford A (top image, both VR; second image, axial MPR) and Stanford B (third image, arterial phase VR, venous phase VR; fourth image, MIP and VR; fifth image, axial MPR). T = true lumen. F = false lumen. Black arrowhead = entry site. All images courtesy of Qi Liu, Ph.D.
   |
In addition, initial entry sites were defined in 105 of 136 cases. In 53 patients, MRA depicted initial entry sites that were confirmed with surgery or angiography. Depiction of these sites was significantly better on VR, VE, and MPR images, Lui said. Volume rendering was particularly useful.
The orifice of anonymous arteries involved in type I dissections was 37%. A little over 10% of the left subclavian artery was involved in type III dissections. In 134 patients with type I and type II dissections, 40.3% of the cases involved the kidney arterial. The celiac arterial was involved in 14.9%, and the super mesenteric arterial in 4.5%.
The initial entry site of Stanford B and its relationship with left subclavian artery (top images, both VR).
 |
Finally, the false lumen with large amounts of thrombi was found in 23.5% of the cases, and complete thrombi in 22.8%.
"The shape, size, and the relationship between the arterial orifice and the initial entry sites were clearly demonstrated with 3D on VR images, which was helpful for surgical and endovascular treatment," the group wrote in their abstract.
 |
Aortic dissection assessment, before (above) and after (below) surgery.
 |
"3D MRA can prove to be the optimal imaging modality for aortic dissection," Liu added.
These results dovetail with other recently published research. In a review article, Japanese radiologists from Yamaguchi University School of Medicine praised MRA for its inherent multiplanar imaging capability and ability to overcome difficulties in visualizing distal branch vessel lesions. They echoed Liu's statement that MRA might "obviate the need for conventional angiography in the near future" (Topics in Magnetic Resonance Imaging, June 2003, Vol. 14:3, pp. 253-266).
More recently, a group from the Uniformed Services University of the Health Sciences in Bethesda, MD, recommended MRA for detecting and monitoring thoracic vascular anomalies in patients with Turner's syndrome, which is associated with aortic coarctation and dissection (Circulation, September 21, 2004, Vol. 110:12, pp. 1694-1700).
By Shalmali Pal
AuntMinnie.com staff writer
December 30, 2004
Related Reading
Classic 2D time-of-flight MRA aids severe carotid stenosis diagnosis, October 18, 2003
Vascular & Interventional Radiology: The Requisites, September 22, 2004
RFCA for afibrillation evolves with MDCT, July 23, 2004
Copyright © 2004 AuntMinnie.com