Patent foramen ovale (PFO) is a known cause of cerebral strokes. Adding insult to injury, studies have shown that the incidence of stroke is even higher if PFO is associated with an atrial septal aneurysm. Of course, the ideal imaging test would diagnose both conditions. Cardiovascular researchers from Europe suggest using contrast-enhanced dynamic MRI for dual detection.
"Until now, the diagnosis of PFO has not been possible using MRI because of insufficient spatial and temporal resolution and the absence of a measurable shunt volume," wrote Dr. Oliver Mohrs and colleagues from the Cardiovascular Center Bethanien in Frankfurt, Germany. "The results presented in this study underline the potential of contrast-enhanced MRI to noninvasively (and) reliably detect PFO either by visual assessment or by computation of signal-time intensity curves" (American Journal of Roentgenology, January 2005, Vol. 184:1, pp. 234-240).
Mohrs' co-authors are from the German Cancer Research Center in Heidelberg, Germany, and the University of Oxford Centre for Cardiovascular Magnetic Resonance in Oxford, U.K.
The group set out to investigate the feasibility of MRI to detect PFO and atrial septal aneurysm, evaluate signal-time curves to diagnose the shunt across the PFO, and compare MR to the gold standard, transesophageal echocardiography (TEE).
The study population consisted of 15 patients with TEE-detected PFO. A dozen of these patients had a history of cerebral events. Five patients without PFO based on TEE made up the control group. TEE was performed with a 5-MHz phased multiplane probe (Vingmed System FiVe, GE Healthcare, Waukesha, WI), 0.02 mg of oral lidocaine, and a 10-mL bolus of Echovist (Schering, Berlin) given during a Valsalva maneuver. Atrial septum aneurysm was defined as a protrusion of greater than 10 mm into the left or right atrium.
MRI was performed on a 1.5-tesla system (Magnetom Sonata Maestro Class, Siemens Medical Solutions, Erlangen, Germany) using 10 mL of Magnevist (Schering AG, Berlin), also administered during a Valsalva maneuver. The protocol included ECG-gated true fast imaging. The presence of atrial septal aneurysm was assessed by a cardiologist and radiologist who were unaware of TEE results. PFO was diagnosed using visual assessment, signal-time curves, and a four-point grading system. Grade 0 meant no contrast enhancement in the left atrium before the contrast agent reached the pulmonary vein. A grade 3 score indicated bright contrast enhancement.
 |
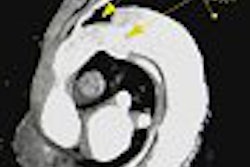
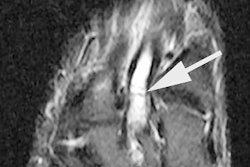
| Thirty-two-year-old man with PFO grade 3 on TEE and grade 3 on MRI. Above and below, images show enhancement of entire left atrium due to right-to-left-shunting (arrows) before enhancement of pulmonary vein. Mohrs OK, Petersen SE, Erkapic D, Rubel C, Schräder R, Nowak B, Fach WA, Kauczor HU, Voigtlaender T, "Diagnosis of Patent Foramen Ovale Using Contrast-Enhanced Dynamic MRI: A Pilot Study" (AJR 2005; 184:234-240). |
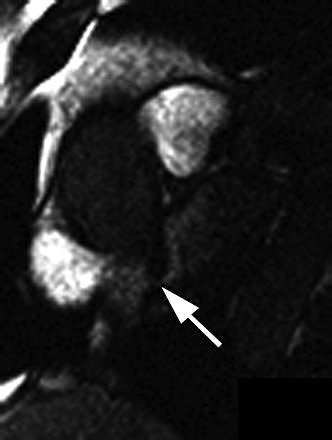 |
The results showed that PFO was visually identified in all 15 patients, and excluded in the control group on MRI. For the patients with PFO, "an early contrast enhancement due to intracardiac right-to-left shunting was present in the left atrium before the contrast agent reached the pulmonary veins," the authors wrote. There was a 20% prevalence of atrial septal aneurysm in the PFO population, and MRI correctly identified these cases.
In terms of grading, 47% of the PFO patients were given grades identical to TEE, and there was no systematic under- or overestimation of the grades. However, this correlation was good as long as all patients (PFO and control) were included. If the patients without PFO were excluded, then the correlation was poor, Mohrs' group stated.
They hypothesized that this discrepancy might be caused by intraindividual variability during the Valsalva maneuver. If the maneuver is performed incorrectly, a PFO can be missed, they added.
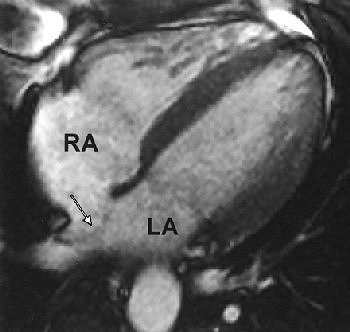 |
| Thirty-two-year-old man with atrial septal aneurysm (arrow) on MRI. Typical bulging of atrial septum is shown toward left atrium in horizontal long axis (LA; RA = right atrium). Mohrs OK, Petersen SE, Erkapic D, Rubel C, Schräder R, Nowak B, Fach WA, Kauczor HU, Voigtlaender T, "Diagnosis of Patent Foramen Ovale Using Contrast-Enhanced Dynamic MRI: A Pilot Study" (AJR 2005; 184:234-240). |
Using the signal-time curves, all PFO patients showed curves with an early first peak in the left atrium of 160% of baseline signal at seven seconds, followed by the peak in the pulmonary vein of 486% at 17 seconds.
"The advantage of signal-time curve analysis is the clear-cut differentiation of contrast enhancement due to right-to-left shunting in the left atrium from pulmonary flow," the authors explained.
While their results were positive, the group said larger prospective studies were needed to confirm their findings. In an interesting aside, they suggested that future studies might also evaluate the feasibility of MRI as a noninvasive screening technique for PFO in scuba divers.
By Shalmali Pal
AuntMinnie.com staff writer
January 14, 2005
Related Reading
Study questions PFO and cerebral damage link in scuba divers, January 14, 2005
Cluster headache linked to patent foramen ovale, October 22, 2004
Heart defect poses scuba diving risk, July 14, 2004
Patent foramen ovale identified in stroke cases related to air travel, June 30, 2003
Copyright © 2005 AuntMinnie.com