SAN FRANCISCO - Cardiac MRI is showing its capabilities as a high-tech crystal ball -- able to predict which heart patients will suffer future adverse events -- in presentations at this week's Society for Cardiovascular Magnetic Resonance (SCMR) meeting.
Researchers in four separate studies examined the modality's performance in predicting events among women with suspected ischemia, patients with symptoms of coronary artery disease (CAD), patients with definite CAD, and patients with reperfused acute myocardial infarctions.
The findings are being presented today at the 8th annual SCMR scientific sessions, with abstracts published in the Journal of Cardiovascular Magnetic Resonance (January 2005, Vol. 7:1).
Researchers from the multicenter Women's Ischemia Syndrome Evaluation (WISE) study have found that a global myocardial perfusion index (GMPi) calculated by MRI, in conjunction with a Framingham risk score, can identify those patients who would benefit from conventional quantitative coronary angiography (QCA).
Using just a Framingham score to risk-stratify patients has proved unsatisfactory because many women with intermediate or higher Framingham risk don't exhibit severe coronary disease at QCA.
The researchers looked at 133 women with suspected ischemia, and divided them into groups based on their GMPi and Framingham scores. They then followed up on the patients for an average of more than three years, and noted all "major adverse cardiovascular events" -- defined as either death or myocardial infarction (MI).
Among the 33% of patients deemed to have neither GMPi nor Framingham risk, none had suffered an adverse event. Meanwhile, those 20% of the women who had both risk variables experienced 70% of the 10 major events, according to the researchers' abstract.
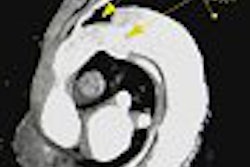
In another study, researchers from Brigham and Women's Hospital in Boston looked at 257 patients who presented with CAD symptoms and underwent cardiac MRI for assessment of myocardial viability or detection of myocardial infarction.
Over a mean follow-up of 13.8 months, there were 54 adverse events among the patients: 30 deaths, three acute MIs, and 21 cases of unstable angina or decompensated congestive heart failure. The presence of myocardial delayed enhancement on a contrast-enhanced MRI was the strongest predictor of those events, the researchers report.
Another group, composed primarily of researchers from the University of California at Irvine and other southern California centers, looked at infarct size in 100 patients. The patients were followed for an average of 25 months, and 15 died during that period.
The size of the infarction -- whether it was greater than 15% of the patient's left ventricular mass -- was the best independent predictor of death. Other variables, such as gender, extent of CAD, prior history of MI, hypertension, and diabetes weren't significant.
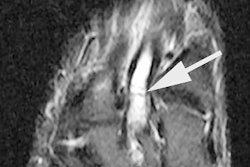
In the fourth study, researchers from Friedrich-Alexander-Universitaet Erlangen-Nürnberg in Erlangen, Germany, looked at 102 patients who had undergone reperfusion of an acute MI. Left ventricular dysfunction was determined by delayed contrast-enhanced MR within 10 days of the reperfusion.
Among the patients there were 11 deaths and reinfarctions over a mean follow-up of 2.5 years. Those adversely affected patients had significantly higher areas of dysfunction, as seen on MR, than those who were unaffected.
Ejection fraction and the dysfunctional-but-viable area as determined by MR were "related to occurrence of future events independent of the presence of risk factors for coronary arteriosclerosis," the researchers concluded.
By Tracie L. Thompson
AuntMinnie.com staff writer
January 21, 2005
Related Reading
MRI touted for SPECT's role in sizing infarcts, August 4, 2004
Cardiac MRI shines in predicting heart attack in women, March 8, 2004
Cardiac MRI outdoes SPECT in spotting microinfarcts, February 14, 2003
Cardiac MRI may improve triage of patients with chest pain, February 4, 2003
Copyright © 2005 AuntMinnie.com