Proton magnetic resonance spectroscopy (MRS) is a powerful analytic and diagnostic tool whose efficacy has been proved in numerous peer-reviewed studies.
However, in a January 2004 decision memo, the U.S. Centers for Medicare and Medicaid Services (CMS) said that it "determined that the evidence is not adequate to conclude that MRS is reasonable and necessary for diagnosis of brain tumors; therefore, we will continue the current national noncoverage determination."
The CMS decision supported earlier conclusions about the use of the modality for brain tumor diagnosis reached by private-payor organizations in the U.S. An assessment program conducted by the Blue Cross/Blue Shield Association on the use of the technology for the evaluation of suspected brain tumor stated that "the evidence is insufficient to permit conclusions concerning the effect of MRS on health outcomes" (Technology Evaluation Center Assessment Program, January 2003, Vol. 18:1).
In a scientific poster presentation at the 2004 RSNA conference in Chicago, a research team from California presented compelling evidence that the use of MRS for brain tumor diagnosis is not only safe and accurate, but cost-effective.
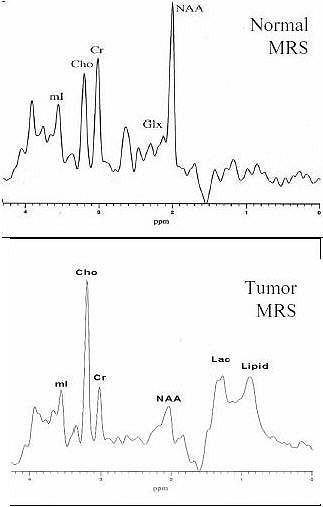 |
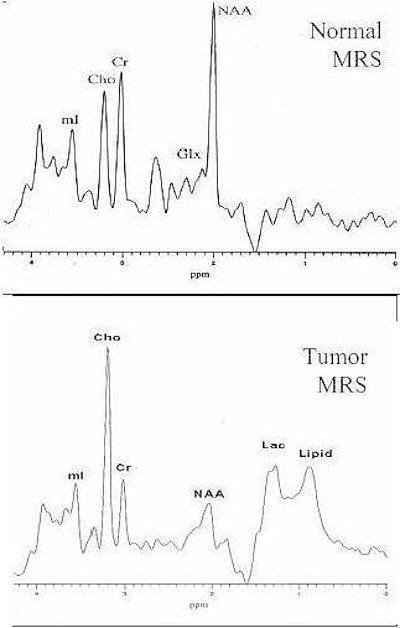
| Increased Cho, decreased NAA, and the presence of lipid and lactate in the spectra give a characteristic pattern for the diagnosis of brain tumor using MRS. Image and caption courtesy of Alexander Lin and the Rudi Schulte Research Institute. |
"I think part of the problem (as to the adoption of MRS for brain tumor diagnosis) has been that this technique has been in the hands of physicists and scientists, and not in the hands of clinicians and radiologists," said Alexander Lin, senior scientist at the Rudi Shulte Research Institute and director of clinical services at the Huntington Medical Research Institutes in Pasadena, CA, who presented the group's research.
According to Lin, a cost-benefit analysis of MRS for brain tumor diagnosis has never been published. By measuring a cost-benefit analysis of MRS in a controlled study, the team sought to answer CMS and payor criticism for the lack of outcomes analysis and the societal impact of the technology for brain tumor diagnosis.
The researchers conducted single-voxel short-echo proton MRS on 14 patients, nine with biopsy-proven tumors and five with suspected tumors, in which a clinician had mapped a diagnostic treatment plan on the basis of patient history and previous tests. The MRS results were then reported to the clinician and factored into the clinical decision-making process, and a final diagnostic and treatment plan was formulated, Lin said.
The diagnostic costs of the initial treatment plan were determined using CPT codes for all elements of the recommended procedures. A billing specialist was consulted to determine costs on the basis of the 50th percentile of medical fees reported in the U.S. for the procedures, the researchers reported. The cost savings were calculated on the basis of savings accrued because of changes in the treatment plan minus the cost (50th percentile of CPT code 76390; $1,200) of a single MRS exam per patient.
In the original treatment plan, stereotactic biopsy (CPT 61750) was recommended in eight cases at a cost of $7,024 per patient (including physician professional fees, length-of-stay costs, operating room costs, anesthesia, guided CT, and pathology). An open craniotomy (CPT 61510) was recommended in three cases at a cost of $8,380 per patient (including physician professional fees, length-of-stay costs, operating room costs, and anesthesia). Additional MRI scans with gadolinium (CPT 70552) were recommended for the other three patients every six weeks at a cost of $2,898 per patient (assuming a minimum of two exams per patient).
In the final treatment plan, seven of eight patients avoided stereotactic biopsy, for a total cost savings of $39,568. Despite the negative MRS results in the eighth patient, the clinician went ahead with the biopsy and found no tumor, resulting in a waste of $8,224 (the biopsy plus the MRS cost) as well as the potential for patient morbidity as a result of the procedure.
In one of three cases, the researchers wrote that MRS diagnosed radiation necrosis and the clinician elected not to resect, avoiding surgery and saving $4,780. In two of the three cases, MRS confirmed the clinical suspicion of a brain tumor and resection was conducted according to treatment plan.
In the three treatment plans that called for repeat MRI exams with gadolinium, the use of MRS resulted in a cumulative cost savings of $5,094.
"MRS can be combined with the initial MR exam, allowing for earlier diagnosis of brain tumor than serial MR scans, quicker treatment, and the potential to avoid tumor growth that may negatively impact on a patient's quality of life," Lin noted.
The researcher's study showed that MRS can be used in clinical practice to avoid unnecessary surgery, as well as to quickly and quantitatively determine a brain tumor diagnosis. In addition to lowering treatment cost, the use of MRS decreases the risk of surgical morbidity, provides for the potential of more effective treatments due to an earlier diagnosis, and can increase the quality of life for the patient. The group believes its results can provide the framework from which a larger prospective study can be established.
"The total cost savings of MRS in the clinical management of these patients was $49,442," Lin said. "Considering that there are over 17,000 new cases of brain tumor diagnosed each year, the extrapolated cost savings of MRS use could be as much as $56 million a year."
By Jonathan S. Batchelor
AuntMinnie.com staff writer
January 28, 2005
For further information on the clinical use of MRS, the Huntington Medical Research Institutes will be holdings its annual Clinical MR Spectroscopy Course in Pasadena, CA, March 11-14 this year. The course combines lectures with hands-on training and one-on-one breakout sessions. The institute can be contacted at 626-397-5840, or via its Web site at www.mrs-hmri.org.
Related Reading
MRSI may be just the "tool" to diagnose bipolar disorder, November 30, 2004
Magnetic resonance spectroscopy predicts outcomes in women with chest pain, June 15, 2004
MRS predicts severity of brain injury in abused infants, June 10, 2004
New MR approach quantifies brain metabolite concentrations, March 6, 2004
Echo-planar MR spectroscopy improves mood in depressed patients, January 5, 2004
Copyright © 2005 AuntMinnie.com