Are radiologists writing reports that clinicians find useful? Two new studies suggest substantial room for improvement, and one of the studies has already been cited in the political debate over who should interpret images.
A commonly used noun in chest x-ray reports -- "infiltrate" -- was judged unhelpful by a majority of 151 physicians surveyed in one new study (Radiology, April 2005; Vol. 235:1, pp 5-8).
"Despite the alacrity with which some radiology practitioners use infiltrate, the term seems to provide little insight into the disease process affecting a given patient," the authors wrote.
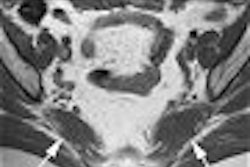
Meanwhile, another new study concludes that orthopedic surgeons should personally review the MRIs of pediatric patients because radiology reports will include "diagnostic inaccuracies" (Journal of Bone & Joint Surgery, March 2005, Vol. 87:3, pp. 497-502).
Dr. Scott Luhmann, an assistant professor of orthopedic surgery at Washington University in St. Louis, MO, led a three-year prospective study comparing the accuracy of radiologists' MRI reports with his own preoperative diagnoses.
Luhmann's predictions, and those of the radiology reports, were compared to findings at arthroscopy in 96 patients ranging from 7.3 to 18.7 years of age.
"The preoperative diagnoses by the surgeon were significantly (p < 0.05) better than the formal interpretation of the magnetic resonance imaging scans by the radiologist for an anterior cruciate ligament tear, a lateral meniscal tear, osteochondritis dissecans, and discoid lateral meniscus," the authors reported.
With ACL tears, for instance, the radiology reports achieved only 74% sensitivity, while Luhmann achieved 100% preoperative sensitivity.
Radiologists have criticized the study, arguing that is flawed because it didn't evaluate the accuracy of musculoskeletal radiologists -- and complaining that Luhmann wasn't blinded to the radiology reports in his preoperative diagnoses.
But Luhmann said the blinding sought by critics was impossible when patients present after their MRIs. "How can I blind myself when my office schedule says 'evaluate ACL tear'?" he asked.
Luhmann also said his intention wasn't to criticize radiologists per se. On the contrary, he was seeking to document that an MRI alone isn't sufficient for diagnosing pediatric knees.
"The difficulty (is) analyzing an MRI with minimal-to-no patient history or exam," Luhmann said. "On a weekly basis, I have adolescents coming into the office with an MRI in hand and a radiologist's interpretation that is incorrect, at least in part."
Therefore, orthopedic surgeons must read the MRIs themselves and not rely on radiology reports, Luhmann said.
Luhmann's conclusions have already been cited by nonradiology specialists testifying before the U.S. Congress against a proposal to limit the provision of high-end imaging to accredited providers.
In the study pertaining to chest x-ray reports, the clinicians surveyed thought the term "infiltrate" referred to an average of six or as many as 14 different pathophysiologies.
"As a clinician, when a radiologist tells me it's an infiltrate, that really doesn't tell me anything," said lead author Dr. Harlan (Steve) Patterson, a pediatric pulmonologist in Washington, DC. "The word infiltrate is really just saying 'shadow.'"
But infiltrate may be a useful term when radiologists and clinicians have a shared understanding of what they are referring to, commented one radiologist.
"When going over films with doctors, many will even ask me 'Does the patient have an infiltrate?' Alas -- I understand that they are asking if the patient has a pneumonia," the radiologist wrote in response to a query from AuntMinnie.com.
In other cases, radiologists may rely on infiltrate when they don't receive enough clinical information to opine on potential pathophysiology, he suggested.
Patterson, however, believes the confusion his survey identified should give radiologists pause. Most pediatric radiologists already eschew use of the term infiltrate, he said.
"I think it really doesn't help the clinician, which is really what you want to do," Patterson said. "That's the end result of what these radiologists do -- help the person at the bedside do the right thing for the patient. I think oftentimes we lose sight of that."
By Tracie L. Thompson
AuntMinnie.com staff writer
April 19, 2005
Related Reading
New tool automates unstructured report analysis, February 18, 2005
Automated report tracking serves clinical, educational goals, January 18, 2005
Rads urged to standardize reporting of vertebral fractures, November 23, 2004
Imaging reports also benefit from improved signal-to-noise ratio, May 3, 2004
Copyright © 2005 AuntMinnie.com