Normal pressure hydrocephalus (NPH) is stirring up controversy. Among those who deal with the condition, disagreement simmers over what causes it, how to treat it, and even the way to diagnose it.
NPH is a condition in which intracranial buildup of cerebrospinal fluid (CSF) causes the ventricles to enlarge and compress brain tissues. NPH causes gait disturbance, incontinence, and dementia. Usually the cause is unknown; such cases are called idiopathic NPH. Educated guesses blame it on trauma, infection, and subarachnoid hemorrhage.
Experts even argue over who originally identified NPH. It's popularly credited to R. D. Adams and colleagues, who described it back in 1965 (New England Journal of Medicine, July 15 1965, Vol. 273, pp. 117-126).
Others claim the designation "normal pressure hydrocephalus" is wrong, claiming that "an abundance of literature based on (intracranial pressure) monitoring ... acknowledges that CSF pressure (in NPH) may actually not be normal" (Journal of Neurology, Neurosurgery, and Psychiatry, July 2002, Vol. 73:1, pp. 9-12).
That said, NPH is the only dementia disorder that is potentially reversible. Ask doctors about it, though, and you may get a different response from each one.
"I think NPH starts out in infancy, as a disease called benign external hydrocephalus," said Dr. William Bradley Jr., Ph.D., chairman of the radiology department at the University of California, San Diego (UCSD). "When I read out MRs or CTs, I see a lot of patients with big ventricles who could very conceivably have pre-NPH. Once they get old enough, with deep white-matter ischemia as the second hit, they're the ones who could go on to develop NPH. They do just fine until they get to be 60 or so, and then the ischemic change puts them over the top, and the two diseases together cause NPH."
"It's one of those entities that has bedeviled us for so long," commented Dr. William Dillon, chief of neuroradiology at the University of California, San Francisco (UCSF). "It's basically a diagnosis based on clinical symptoms and syndromes. This is different than, say, obstructive hydrocephalus. The ventricles may be slightly enlarged, but often in the range of normal for an elderly person, and it just becomes a very difficult diagnosis to differentiate from atrophy."
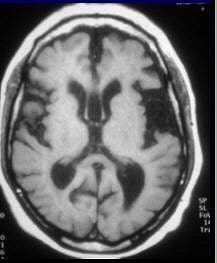
 |
| "Normal pressure hydrocephalus is remarkable for two reasons: (1) It is one of the few treatable causes of dementia, and (2) neuroradiologists are usually involved in making the diagnosis," commented Dr. William Bradley Jr., Ph.D., in the American Journal of Neuroradiology. Image courtesy of Dr. William Bradley Jr., Ph.D. |
"Someone who has Alzheimer's disease may have big ventricles, but they also have enlarged sulci, the spaces over the surface of the brain," added Dr. Jeffrey Petrella, associate professor of radiology in the neuroradiology division of Duke University Medical Center in Durham, NC. "In patients who have a lot of cortical atrophy, that space becomes large because of loss of tissue. What suggests the diagnosis of NPH is that the ventricles are big, but the sulci are not prominent."
When it comes to imaging NPH, the experts continue this spirited debate. The only thing anybody agrees on is that NPH is underdiagnosed. Why? Media overexposure of Alzheimer's disease (AD) has ensured its stature as the diagnosis of choice among doctors examining dementia patients.
Dr. Sean Lilienfeld is vice president of clinical research and regulatory affairs at Codman & Shurtleff, and a 20-year veteran in the dementia field. Codman, a division of Johnson & Johnson, manufactures central nervous system disorder devices. The company currently has a Web site that draws consumer attention to NPH.
"A lot of elderly patients are managed by primary care physicians who are more likely to think first of common diseases. When referring patients for special investigations and scans, they may say, "I think this patient's got Alzheimer's disease,'" Lilienfeld said. "And unfortunately, it tips the scale. (AD and NPH) films are not that dramatically different. The radiologist may then word his report in a way that confirms what the primary care physician originally said about Alzheimer's disease. And that's the problem."
Modalities on parade
Nearly all modalities are used in diagnosing NPH. MRI, CT, angiography, scintigraphy, and ultrasound (on infants) are used to confirm enlarged ventricles and white-matter ischemia.
Cisternography, which involves injecting a radionuclide into the subarachnoid space and following it over a period of hours with CT, MRI, or gamma camera, is used to evaluate CSF absorption. And Dr. Maria Mataró and colleagues proved SPECT has value in assessing postsurgical cerebral perfusion improvement (Journal of Nuclear Medicine, December 2003, Vol. 44:12, pp. 1884-1889).
Bradley was among the first to do the same with MRI. He said he preferred MRI because it gives additional flow information. In a commentary in the American Journal of Neuroradiology, Bradley wrote: "A number of groups have noticed an increased incidence of subcortical, deep white-matter hyperintensities on T2-weighted MR images" (AJNR, October 2000, Vol. 21:9, pp. 1586-1641).
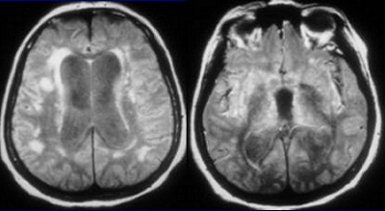
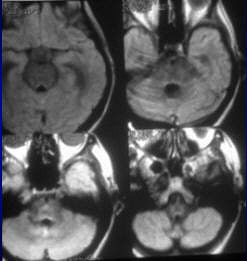
 |
| Seventy-eight-year-old female patient evaluated for suspected NPH. A and B, MRI FLAIR sequence (1 tesla, TR 11,000 msec, TE 140 msec, TI 2,600 msec) shows dilatation of the ventricles and sylvian fissures. C and D, FLAIR after 100% O2 for five minutes shows increased SI in the sulci and the posterior aspects of both sylvian fissures, allowing visualization of hypointense cysts (arrows) due to neurocysticerosis more anteriorly within the sylvian fissures. Note that there is no increase in the SI of the CSF within the ventricles. Braga FT, da Rocha AJ, Filho GH, Arikawa RK, Ribeiro IM, and Fonseca RB, "Intensity of CSF Depicted by Fluid-Attenuated Inversion Recovery Imaging," (AJNR, 24:1863-1868, October 2003). |
At the time of his AJNR commentary, Bradley was at Memorial Medical Center in Long Beach, CA. There, a routine MR scan using conventional (not fast spin-echo) protocol was performed if the patient had NPH symptoms. At UCSD, the MRI protocol for NPH is fast spin-echo imaging followed up with a phase-contrast CSF flow study. The latter is done because fast spin-echo is less sensitive to the flow void, Bradley told AuntMinnie.com.
Dillon agreed that MRI can be useful, but cautioned there's no gold standard for NPH. "We're never really sure of the diagnosis or the outcome," he said. "You're dealing with a population that is, at best, poorly characterized."
Writing in AJNR, Dillon stated that "MR imaging is essential to establish the presence of ventricular dilatation and to exclude other conditions that also may be responsible for the clinical triad of gait disorder, mental slowing, and urinary incontinence."
However, he and co-author Dr. Robert Fishman from UCSF added that a major issue overlooked with MR is "whether the ventricular enlargement observed is consonant with the degree of enlargement of the cortical sulci" (AJNR, October 2001, Vol. 22:9, pp. 1640-1641).
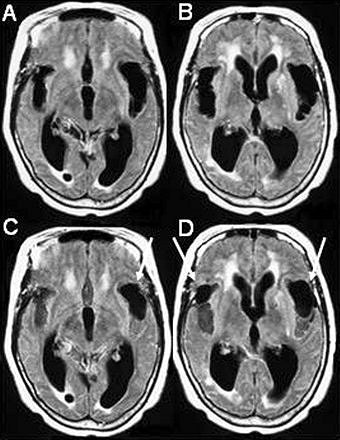
 |
| A simple regression analysis between the SPECT images for each subject (and condition) and the NPH scores showed a positive relationship in Brodmann's area 32, corresponding to the anterior cingulate, and the frontal part of the left lobule of the insula of Reil. Image shows two areas most related to clinical improvement from regression analysis. Reprinted with permission from the Society of Nuclear Medicine. Mataró, M; et al, "Postsurgical Cerebral Perfusion Changes in Idiopathic normal pressure hydrocephalus: A Statistical Parametric Mapping of Study of SPECT Images" (J Nucl Med 2003; 44:1884-1889, Fig. 3, p. 1888). |
Petrella said he preferred functional imaging. "Structural imaging such as CT and MRI can indicate the possibility of normal pressure hydrocephalus, but 111indium nuclear cisternogram is a more specific test for that. Some patients will have a fluoroscopically guided lumbar puncture (with a radionuclide). Then they're imaged a number of hours later with a gamma camera."
So who's interpreting all these images?
"Most of it is done by a mishmash of neuroradiologists and general radiologists," Dillon said. "At (UCSF), a neuroradiologist reads them. It depends on the practice, but an NPH patient wouldn't normally come to a hospital, where the neuroradiologists are."
Widespread confusion
"There's no question that NPH exists," Dillon said. "The issue will always be: Who really has it?"
Industry sources generally agree that NPH accounts for 2% to 10% of all dementias. Guesses about exact numbers, however, vary. The American Association of Neurological Surgeons estimates 250,000 Americans have NPH. Others estimate the number of U.S. cases ranges from 200,000 to 750,000, according to the National Council on the Aging.
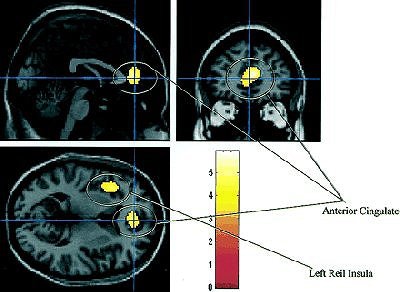
 |
| Enlarged sylvian cisterns in NPH. Studies have indicated that the sylvian CSF volume in patients with idiopathic NPH is significantly greater than in patients with Alzheimer's disease (AJNR, August 1998, Vol. 19:7, pp. 1277-1284). Image courtesy of Dr. William Bradley Jr., Ph.D. |
NPH is often misdiagnosed as degenerative dementias, particularly Parkinson's and Alzheimer's diseases. Subsequently, NPH is mischaracterized as a condition that afflicts only the elderly, when in fact it can occur in a pediatric population. And it's often erroneously called a "curable dementia," which is inaccurate, according to Dr. Philippe Bret and colleagues from the Hôpital Neurologique et Neurochirurgical Pierre Wertheimer in Lyon, France.
"Such confusing terms have generated the widespread myth that some forms of 'true' dementia can be cured by shunt surgery.... This erroneous belief abusively led to extensive application of shunt operations in demented patients, with uniformly devastating results," they wrote in the Journal of Neurology, Neurosurgery, and Psychiatry (July 2002, Vol. 73:1, pp. 9-12).
The trouble with shunts
After 50 years, the efficacy of shunts is still hotly debated. The success rate of shunts averages 50%. "Response to shunting seems to be worse (30-50%) for patients with the idiopathic form (of NPH) than for patients with a known case of communicating hydrocephalus (50-70%)," Bradley wrote in his AJNR commentary.
In his editorial, Bret added that "nowadays, neurosurgeons are occasionally requested to use shunting in (dementia) patients based on the argument that 'they have nothing to lose.'"
One recent study even concluded that there is no proof that NPH shunts are effective because there are no randomized, controlled trials that compare shunted patients to those who do not undergo shunting (Cochrane Database of Systematic Reviews, 2005, Issue 1; 2002, Issue 3: CD003157).
 |
| The advantage of using MRI to track NPH is that imaging can be done in any plane. MR is also more sensitive to interstitial, transependymal flow of cerebrospinal fluid, and hyperdynamic CSF flow seen with shunt-responsive NPH, as seen above (Neurosurgery Clinics of North America, October 2001, Vol. 12:4, pp. 661-684, viii). Image courtesy of Dr. William Bradley Jr., Ph.D. |
However, a team from Finland conducted a prospective study of 51 NPH patients, and found that 32% of the patients who had received shunts had died after five years, compared with 35% of the unshunted patients who had died (Acta Neurochirurgica, June 2002, Vol. 144:6, pp. 515-523).
MRI is the modality of choice for following shunt implantation, although it does have its drawbacks. In a study of 168 patients fitted with noninvasively programmable valves, half the devices required postoperative reprogramming after MRI exposure (Journal of Neurosurgery, July 1999, Vol. 91:1, pp. 26-31).
Shunt manufacturer Sophysa of Orsay, France, states that the majority of its hydrocephalic valves are MR-safe, up to 3 tesla. But when any valve goes out of whack, it must be reprogrammed, which is usually done by the neurosurgeon that implanted it.
Other problems with shunts include infections, overdrainage, obstructions caused by tissue plugs or blood clots, and separation or failure of components.
"When you shunt older patients, they can sometimes develop subdural hematomas and go downhill. So there's a fair amount of risk involved, particularly if you shunt a patient who doesn't have NPH," Dillon said.
Petrella and Bradley agreed. "You don't proceed to a shunt unless the gait problem is really bad," Bradley said.
Dementia dollars
It's probably no coincidence that most of the so-called educational information available about NPH comes from pharmaceutical companies looking to reach out and shunt someone. Their Web sites helpfully offer self-evaluation tests full of red flags -- "trouble remembering things," "forgetting names or appointments" -- that encourage people to seek help immediately.
How lucrative can the business of NPH ultimately be? In the U.S. alone, $100 billion is spent annually on treating AD. If AD cases represent 70% of all dementia cases and NPH 2% to 10%, then NPH is potentially a $2.85 billion to $14.3 billion market.
According to Frost & Sullivan pharmaceuticals analyst Dhiraj Ajmani, hydrocephalus shunts were a $53.6 million market in 2004, but "the growing acceptance of pressure-adjustable valves, which are triple the price of fixed-pressure valves, is expected to spur revenues."
The National Council on the Aging claims that currently only 11,500 NPH patients in the U.S. are shunted annually; Codman's Lilienfeld says it's more like 20,000. Either way, that still makes it a wide-open market for anyone with designs on rapidly graying baby boomers.
"Offering someone a potentially curable cause for dementia is a very appealing thing," Petrella said. "But the other side of the coin is that you don't want to overidentify these people, and put shunts in everybody."
By Sydney Schuster
AuntMinnie.com contributing writer
March 24, 2005
Related Reading
Low bone mineral density linked to Alzheimer's disease risk, January 27, 2005
Functional MRI: Advancing clinical opportunities for neuroradiology, November 8, 2004
Enlarged perivascular spaces linked with worse cognitive function, October 29, 2004
Copyright © 2005 AuntMinnie.com