If there's only an MRI diagnosis of partial thickness rotator cuff tear (PTRCT), the shoulder surgery should probably wait. That's the upshot of two studies that also serve as reminders of inherent and practical limitations of diagnostic imaging in particularly difficult-to-visualize scenarios.
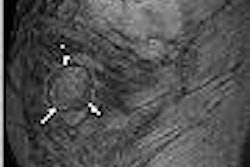
The inherent limitations of MRI and ultrasound in PTRCT are referenced in a new study in the American Journal of Radiology, led by Dr. Sharlene Teefey from the Mallinckrodt Institute of Radiology in St. Louis (AJR, June 2005, Vol. 184:6, pp. 1768-1773).
The researchers sought to analyze the causes of sonographic errors in detecting rotator cuff tears in 71 consecutive patients, and found that partial-thickness tears were particularly problematic. Diagnostic errors were made in six of the 19 partial-thickness tears, compared to just one error in the detection of 46 full-thickness tears.
Because all of the patients had also undergone shoulder MRI as part of another study, the authors noted that "many of the cases that were problematic for sonography were also problematic for MRI."
"This primarily reflects the difficulty that both tests have in distinguishing extensive partial-thickness or large bursal-side tears from full-thickness tears and tendinopathy from partial-thickness tears," the authors wrote.
That said, the authors also played down the significance of these inherent imaging difficulties.
"Clinically, a failure to distinguish extensive partial-thickness from full-thickness tears may not be important because orthopedic surgeons generally treat extensive partial-thickness tears or large bursal-side tears as if they were full-thickness ones," the authors wrote.
The distinction between partial-thickness tears and tendinopathy, they added, "may not be clinically relevant because both are initially managed nonoperatively."
Meanwhile, the practical limitations that may further diminish MRI diagnoses made in community settings were reflected recently in a study by Dr. Stephen Weber, who practices with Sacramento Knee & Sports Medicine in California.
In a presentation at the American Academy of Orthopaedic Surgeons (AAOS) meeting in February, Weber said his goal was to caution colleagues against the increasingly common practice of scheduling patients for surgery based solely on an MRI report.
"What happens classically is you sign the patient up for surgery, you don't do any workup other than the MRI scan, you get in there, and there's nothing there," Weber said. "You're standing there with a scope going 'Great, what do I do now?'"
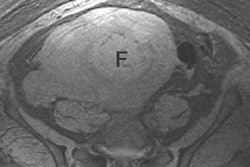
Weber's study looked prospectively at 80 consecutive patients who presented to his practice with an MRI diagnosis of PTRCT and who ultimately underwent arthroscopy after conservative management of their symptoms failed.
Patients were initially treated based on clinical findings using Neer's algorithm and lidocaine impingement tests. Arthroscopy was presumed to be the gold standard for diagnosis, and all of the arthroscopic exams were videotaped.
The weakness of MRI in this area was evident even prior to arthroscopy, as 65% of the scans were reported as "possible" partial tears. At arthroscopy, MRI predictions of PTRCT turned out to be accurate in only 17 (22%) of the patients.
Twenty-five patients (31%) without PTRCT had what Weber deemed to be complete rotator cuff tears, and 47% had no tear at all. Ten percent turned out to have calcific tendinitis rather than a partial tear.
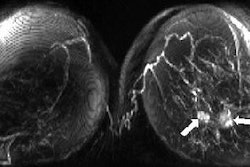
Weber found that the use of fat-suppression techniques apparently didn't aid the diagnosis. Only eight of 33 scans performed with fat suppression had correct diagnoses.
Also, scanning at a higher field strength didn't improve performance. Ten of the 30 lower-field MR scans resulted in a correct diagnosis versus 13 of the 50 standard 1.5-tesla MR scans.
The impact of contrast enhancement on accuracy could not be analyzed because only five of the scans included contrast, Weber noted. No overall sensitivity or specificity was calculated because no PTRCT-negative MR scans were taken to arthroscopy as part of the study.
"In my opinion, the reading of a partial thickness cuff tear on MRI is not clinically useful. Too many false positives, missed a lot of complete tears, and 47% were not torn at all. Twelve percent of these patients did not clinically have impingement," Weber said.
"The common surgical practice of urgent surgery for the MRI reading of a partial thickness cuff tear, with an incidental acromioplasty and arthroscopic exploration that is negative, is a seriously flawed concept," Weber concluded.
By Tracie L. Thompson
AuntMinnie.com staff writer
June 17, 2005
Related Reading
Enthesopathy on shoulder MRI may tag severity of rotator cuff tears, February 24, 2005
Acromion evaluation proves tricky for x-rays and MRI, February 21, 2005
Standard and extremity MR bear brunt of shoulder imaging, November 17, 2004
Shoulder finding may aid in detection of ankylosing spondylitis, November 15, 2004
Copyright © 2005 AuntMinnie.com