The 6657 trial currently under way at the American College of Radiology Imaging Network (ACRIN) will scrutinize contrast-enhanced MR for evaluating breast cancer patients treated with neoadjuvant therapy. As of June 6, ACRIN 6657 had 177 of a target goal of 244 enrollees.
In the meantime, two studies in the American Journal of Roentgenology offer a preview of how well breast MR fares in postchemotherapy treatment patients. The first study from France assessed washout volumes and its potential relationship to vascular conditions. The second study determined if MRI measurements of breast tumor volume could predict recurrence-free survival.
MR washout
"The exact significance of washout is unclear. Its presence appears to be related to various vascular conditions," wrote Dr. Carl El Khoury and colleagues from the Institut Curie in Paris. They hypothesized that "washout quantification may constitute a surrogate for microvessel counting with immunohistochemical techniques that requires repeat biopsy" (AJR, May 2005, Vol. 184:5, pp. 1499-1504).
For this study, 19 patients with pathologically proven breast cancer were enrolled. All were treated with neoadjuvant chemotherapy, surgery (lumpectomy or mastectomy), and radiation therapy. Three gadopentetate dimeglumine-enhanced MR exams were performed: before surgery, after the second course of chemotherapy, and after the last course. The protocol consisted of five data acquisition series, but only the dynamic sagittal series was analyzed to produce parametric images representing washout pattern.
Cutoff values and tumor washout volumes were recorded by two radiologists, with three volumes obtained per patient:
- Volume 1 -- before chemotherapy
- Volume 2 -- during chemotherapy
- Volume 3 -- before surgery
The results showed that the mean greatest axis of enhancement on the first MR studies was 47 mm in 19 cases. A significant decrease of the washout volume was observed after two courses of chemotherapy, but not between two and four courses, El Khoury's group stated.
Reader one came up with the following mean volume measurements:
- Volume 1 -- 1.26 mL
- Volume 2 -- 1.1 mL
- Volume 3 -- 1.1 mL
Measurements for volumes 1-3 for reader two were 3.7 mL, 1.1 mL, and 0.9 mL, respectively. The authors stated that the quantification method for the washout changes had good interobserver agreement, as well as excellent intraobserver agreement.
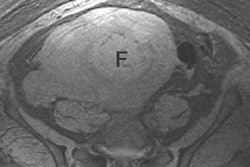
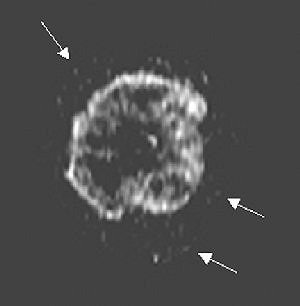
 |
| Forty-five-year-old woman with 3-cm clinical lesion in lower quadrants of breast. Late postcontrast sagittal T1 fast spoiled gradient-echo image shows peripheral decrease of signal (arrows). |
"The mean residual washout in the 16 (pathologically classified) nonresponders was 48%.... In two cases of major response, the residual washout was 0% to 2%. No residual washout was present in the complete responder case," the authors wrote.
The authors pointed out that avoiding motion artifacts was one key to the success of this technique. Indeed, their original patient population was bumped down from 22 because of motion artifacts.
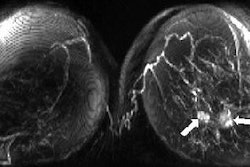
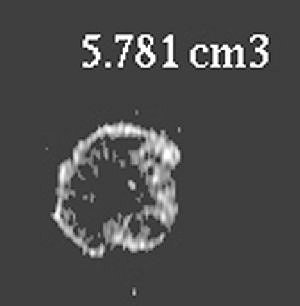
 |
Same patient. Above, parametric washout image shows tumor is isolated from rest of breast. Surrounding pixels (arrows) correspond to washout value smaller than 23 (i.e., cutoff value chosen by observer) and were there excluded from volume processing. Below, applying cutoff and processing volume of remaining pixels resulted in this parametric washout image. El Khoury C, Servois V, Thibault F, Tardivon A, Ollivier L, Meunier M, Allonier C, Neuenschwander S, "MR Quantification of the Washout Changes in Breast Tumors Under Preoperative Chemotherapy: Feasibility and Preliminary Results" (AJR 2005; 184:1499-1504).
 |
This technique can be integrated into a routine dynamic study without more sequencing, such as T1 mapping or more contrast agent. In addition, the parametric view shows all regions of the breast with a decrease of enhancement after a maximum point. Finally, washout quantification can be performed without the placement of regions of interest (ROI), thereby reducing operator dependence, the authors stated.
Tumor volume on MR
A clear advantage of preoperative chemotherapy is that it shrinks larger tumors, enabling more accurate breast conserving surgery. So identifying surrogates that can predict outcome to therapy early would be valuable for tailoring treatment.
"We hypothesize that measurements of tumor volume, calculated by automated segmentation of MRI images, characterize lesion extent more accurately than diameter measures, and may thus prove more sensitive," wrote lead author Dr. Savannah Partridge in the introduction to her group's study (AJR, June 2005, Vol. 184:6, pp. 1774-1781).
At the time of the study, Partridge was at the University of California, San Francisco (UCSF). She is now at the University of Washington in Seattle. Co-authors Nola Hylton, Ph.D., and Dr. Laura Esserman from UCSF are the principal investigators for ACRIN 6657.
The patient population consisted of 62 women (later reduced to 58 when four patients were omitted) with stage II or III locally advanced breast cancer. The women underwent gadopentetate dimeglumine-enhanced MRI before treatment, after one cycle of chemotherapy, and at the completion of treatment, prior to surgery.
Of their protocol, the researchers explained that "fat suppression was an important imaging requirement for discriminating enhancing lesions from bright fat signal on T1-weighted images." They achieved this by using a frequency-selective inversion recovery preparatory pulse that eliminated the fat signal before image acquisition. An in-house, semiautomated software algorithm was applied to segment tumors in 3D MRI datasets.
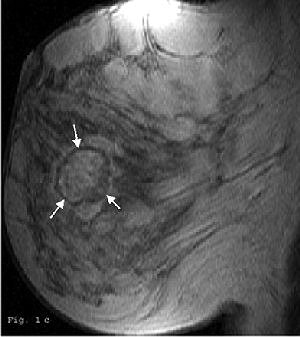
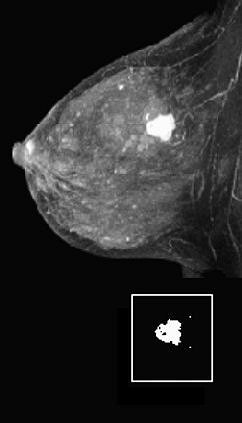
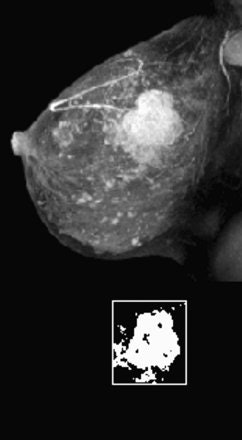 |
Fifty-year-old woman with invasive ductal carcinoma, grade III, studied while undergoing neoadjuvant chemotherapy treatment. MRIL was performed using contrast-enhanced 3D fast gradient-recalled echo-pulse sequence. Patients presented with 22 cm3 (4.7-cm diameter) tumor. Significant reduction in MRI volume was evident after one cycle of chemotherapy (30% decrease) and by end of treatment (88% decrease). Patient had 2.2 cm of residual disease and one involved lymph node at surgery, and continues to be disease-free 20 months after surgery.
 |
According to the results, the most recent follow-up for 58 patients showed 13 cases of local or metastatic disease, with a median time of 10 months to recurrence. After surgery, 45 women remained disease-free (median follow-up of 32.5 months). The median tumor size on MRI was 5.2 cm in diameter before chemotherapy. At surgery, seven of 58 women had complete pathologic responses. The diameter of residual disease in the remaining patients was 2.8 cm.
The investigators found that initial MRI volume was the strongest predictor of recurrence-free survival (RFS). In addition, final change in MRI volume was more predictive than change in tumor diameter. Early change in MRI volume and diameter after one chemotherapy cycle showed a trend toward recurrence-free survival.
"The group with 50% or greater reduction in MRI tumor volume showed significantly longer RFS compared with those with less tumor shrinkage during treatment," they wrote. "Our study indicates that one-dimensional characterization of tumor response may be less sensitive than 3D volume measurements."
The strength of 3D volume measurement is its ability to show the extent of irregularly shaped tumors, multifocality, and diffuse shrinkage during treatment, they added.
By Shalmali PalAuntMinnie.com staff writer
June 14, 2005
Related Reading
Chemohormonal therapy reduces long-term breast cancer mortality, May 13, 2005
Breast MRI OK immediately following biopsy, May 3, 2005
Neoadjuvant and adjuvant therapy generally comparable for breast cancer, February 2, 2005
Scintimammography catches chemoresistance in breast cancer patients, June 13, 2002
Copyright © 2005 AuntMinnie.com