AI-directed stratified MRI scanning could help decrease scan times in breast imaging settings, suggest findings published June 3 in Radiology.
In a simulation study headed by a team led by Sarah Eskreis-Winkler, MD, PhD, from the Memorial Sloan Kettering Cancer Center in New York, AI-directed scanning triaged about 50% of breast MRI exams to an abbreviated breast MRI protocol while maintaining high diagnostic performance.
“These findings herald a new era of AI-directed MRI scanning, where the acquisition plan is not static but changes in real time, as information is acquired and analyzed,” Sarah Eskreis-Winkler and co-authors wrote.
Abbreviated MRI continues to be explored in imaging settings as a potential way to address one of the current limitations of conventional MRI, longer scan times. Studies have shown that abbreviated MRI can produce images that rival the quality of images from conventional MRI scans.
Furthermore, radiologists continue to investigate how deep learning tools could help further streamline breast imaging protocols.
Rather than use AI to sort through worklists or remove low-suspicion exams, the Eskreis-Winkler team repurposed an AI triaging tool to decide which breast MR images should be acquired on a case-by-case basis.
The tool made an “on-the-fly midscan decision” about whether to end the exam at a certain point or continue with the full protocol through a suspicion scoring threshold. Exams with suspicion scores under the 50th percentile were read using both abbreviated and full MRI protocols.
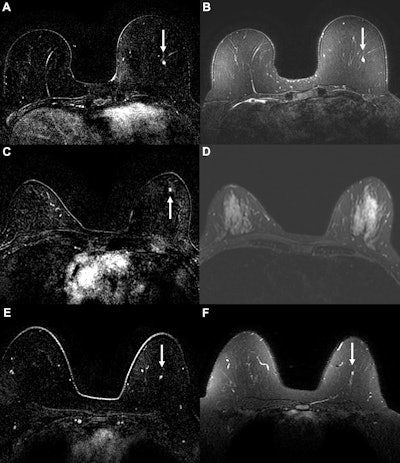 Example cancer examinations where the AI suspicion score prompted triage to abbreviated breast MRI, but readers still assessed the abbreviated MRI exam as suspicious. Axial (A) dynamic contrast-enhanced (DCE) and (B) fat-saturated T2-weighted MRI scans in a 58-year-old woman with a 0.3-cm enhancing focus (arrow) in the left breast. The AI tool generated a suspicion score of 0.68 (43rd percentile of suspicion score), prompting triage at the 50% threshold. For abbreviated MRI, readers gave the examination a suspicious assessment, but for the full MRI protocol, readers missed the suspicious finding, possibly owing to its T2 hyperintensity. The original radiologist also gave a benign assessment, but cancer was diagnosed six months later via mammography, with calcifications indicating ductal carcinoma in situ. Axial (C) DCE and (D) fat-saturated T2-weighted MRI scans in a 51-year-old woman with a 0.3-cm enhancing focus (arrow in C) in the left breast. The AI tool generated a suspicion score of 0.42 (17th percentile), prompting triage at the 50% threshold. For both abbreviated and full MRI, readers gave the examination a suspicious assessment, although the original radiologist report gave a benign assessment. Cancer was diagnosed six months later via mammography. Biopsied calcifications indicated ductal carcinoma in situ. Axial (E) DCE and (F) fat-saturated T2-weighted MRI scans in a 49-year-old woman with a 0.4-cm enhancing focus (arrow) in the left breast. The AI tool generated a suspicion score of 0.62 (37th percentile), prompting triage at the 50% threshold. The lesion was missed by readers at both abbreviated and full MRI. The patient was diagnosed with invasive ductal carcinoma six months after an abnormal contrast-enhanced mammogram.RSNA
Example cancer examinations where the AI suspicion score prompted triage to abbreviated breast MRI, but readers still assessed the abbreviated MRI exam as suspicious. Axial (A) dynamic contrast-enhanced (DCE) and (B) fat-saturated T2-weighted MRI scans in a 58-year-old woman with a 0.3-cm enhancing focus (arrow) in the left breast. The AI tool generated a suspicion score of 0.68 (43rd percentile of suspicion score), prompting triage at the 50% threshold. For abbreviated MRI, readers gave the examination a suspicious assessment, but for the full MRI protocol, readers missed the suspicious finding, possibly owing to its T2 hyperintensity. The original radiologist also gave a benign assessment, but cancer was diagnosed six months later via mammography, with calcifications indicating ductal carcinoma in situ. Axial (C) DCE and (D) fat-saturated T2-weighted MRI scans in a 51-year-old woman with a 0.3-cm enhancing focus (arrow in C) in the left breast. The AI tool generated a suspicion score of 0.42 (17th percentile), prompting triage at the 50% threshold. For both abbreviated and full MRI, readers gave the examination a suspicious assessment, although the original radiologist report gave a benign assessment. Cancer was diagnosed six months later via mammography. Biopsied calcifications indicated ductal carcinoma in situ. Axial (E) DCE and (F) fat-saturated T2-weighted MRI scans in a 49-year-old woman with a 0.4-cm enhancing focus (arrow) in the left breast. The AI tool generated a suspicion score of 0.62 (37th percentile), prompting triage at the 50% threshold. The lesion was missed by readers at both abbreviated and full MRI. The patient was diagnosed with invasive ductal carcinoma six months after an abnormal contrast-enhanced mammogram.RSNA
Final analysis included retrospective data collected from 863 women with an average age of 52 years and 1,423 MRI exams. Of the total, 51 women received a breast cancer diagnosis within 12 months of screening.
The AI-directed stratified scanning that triaged 50% of exams to abbreviated MRI performed well versus conventional MRI.
| Comparison between conventional MRI, AI-directed triaging to abbreviated MRI protocol | ||
| Measure | Conventional MRI | AI-directed triaging to abbreviated MRI |
| Sensitivity | 86.3% | 88.2% |
| Specificity | 81.4% | 80.8% |
| Positive predictive value 3 (percentage of biopsies yeilding cancer) | 24.7% | 23.6% |
| Cancer detection rate (per 1,000 exams) | 30.9 | 31.6 |
| Interval cancer rate (per 1,000 exams) | 4.9 | 4.2 |
The team also noted that the specificity decreased by no more than 2.7 percentage points with AI triaging. It also reported no AI-triaged exams for which conducting the full MRI protocol would have resulted in more cancers detected.
This approach could shorten scan times in patients who do not need images from extra sequences, the study authors highlighted.
“Alternatively, this approach could be applied as a safety check at centers that already offer abbreviated breast MRI, thus averting situations where the radiologist must ask the patient to return for additional MRI sequences,” they wrote. “It also represents an early step in a broader initiative to personalize MRI acquisition on the basis of the initial data acquired during the examination.”
In an accompanying editorial, Fredrik Strand, MD, PhD, from Karolinska University Hospital in Solna, Sweden, called the study results “an important step toward adaptive, efficient, and patient-centered imaging workflows.” He added that this could make way for broader use of AI-based imaging strategies.
“As radiology continues to evolve along with machine learning, such innovations will be essential to improve access, reduce costs, and maintain diagnostic excellence in high-volume screening contexts,” Strand wrote.
The full study can be read here.