An AI-based decision support tool could reduce unnecessary biopsies of benign breast lesions by about 60%, according to research presented December 4 at RSNA 2025.
In his talk, Michael Fishman, MD, from Mass General Brigham and Harvard Medical School in Boston, MA, shared results from his team’s findings showing that the AI tool for breast ultrasound maintained high sensitivity for detecting malignancies while identifying benign lesions.
“The study demonstrates that this tool has the potential to … serve as a reliable pathway toward lowering patient anxiety and expenses, as well as reducing the operational burden on breast imaging practices,” Fishman said.
It remains challenging to accurately diagnose a breast malignancy on an ultrasound. Reports suggest that between 60% and 80% of breast biopsies performed in the U.S. result in benign pathology, adding unnecessary cost and burden to patients, as well as procedural morbidity.
Fishman said this highlights a need for improved diagnostic specificity. He and colleagues evaluated the potential impact of an AI tool (Koios DS, Koios Medical) cleared by the U.S. Food and Drug Administration (FDA) for breast ultrasound. The researchers conducted their prospective study in 2025 at two academic medical centers.
Fourteen fellowship-trained breast imaging radiologists volunteered to participate in the study. Their respective experiences ranged from one to 31 years.
The radiologists documented cases categorized as BI-RADS 4 with a recommendation for ultrasound-guided biopsy, along with the corresponding AI output. All women underwent ultrasound-guided core biopsy, ultrasound-guided aspiration, or surgical excision. Final histopathology served as the reference standard.
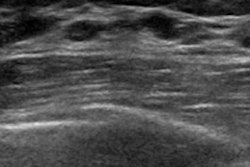
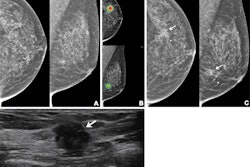
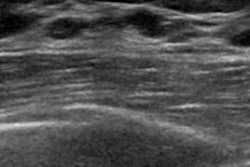
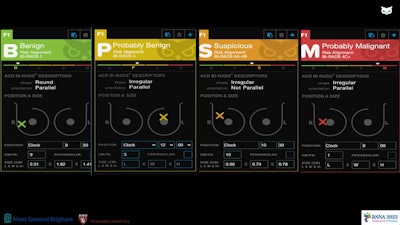 A study presented at RSNA 2025 showed the potential of an AI decision support tool to reduce unnecessary breast biopsies by about 60%. The images shows how the tool flags breast ultrasound findings.
A study presented at RSNA 2025 showed the potential of an AI decision support tool to reduce unnecessary breast biopsies by about 60%. The images shows how the tool flags breast ultrasound findings.
The study included 271 lesions found in 253 women. Of the lesions, 76.8% were benign, while the remaining 23.2% were malignant. The AI tool achieved a specificity of 60.6%, assigning 87 of the benign lesions as BI-RADS 2 and 39 benign lesions as BI-RADS 3.
The AI tool also achieved a sensitivity of 90.5%, but Fishman noted that it incorrectly classified six lesions as malignant. These lesions ranged from 6 mm to 9 mm in size, and five of these lesions had mammographic or MRI correlates.
“[This] highlights a key difference that the AI tool is based solely on the ultrasound features, whereas we as radiologists are also integrating clinical history and multi-modality imaging information to make our final biopsy decision,” Fishman said.
With this in mind, the decision-support tool should not be used as a standalone triage mechanism, he added.
“The takeaway here is that we need to be careful in considering clinical implementation of any of these tools, and ideally it would be used in combination with our own management decision as the final arbiter,” Fishman said. “If that happens, sensitivity could reach 100%.”
He said future work will include prospective evaluation of real-time AI use, the tool’s use in varied practice settings and levels of reader experience, and implications toward cost and revenue.