Functional MRI (fMRI) is not only feasible for fetal cardiac imaging, it can add to clinical perinatal management, according to a group from the Children's Hospital of Philadelphia and the University of Pennsylvania.
Fetal echocardiography has been the main modality in fetal cardiac assessment, but because it is not a true 3D imaging technique, the assessment of ventricular volumes and mass is limited, according to Dr. Mark Fogel and colleagues. While other forms of MRI have been successfully used for imaging in utero, fMRI has proved more difficult.
"Functional fetal cardiac MRI ... has not been performed because triggering to the fetal heart beat, a conceptual necessity for cardiac imaging, has been impossible," wrote Fogel, who is from the hospital's division of cardiology. His co-authors are from the university's anesthesia department, as well as the hospital's Center for Fetal Diagnosis and Treatment (Fetal Diagnosis and Therapy, September-October 2005, Vol. 20:5, pp. 475-480).
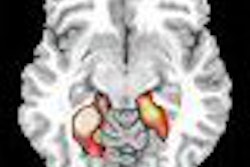
The investigators presented two cases in which they achieved success with fMRI: a fetus with a left diaphragmatic hernia and cardiac compression (mother was 34.5-weeks pregnant at time of fMRI), and another fetus with ductus arteriosus constriction, right ventricular (RV) dilation, and hypertrophy (mother was 36-weeks pregnant).
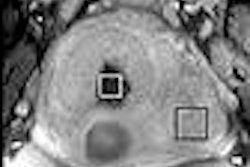
For the fMRI exams, diazepam and morphine were administered intravenously to sedate the fetus. Whole-body MR was performed on a 1.5-tesla scanner (Sonata, Siemens Medical Solutions, Malvern, PA). Body array and spine coils were used. The imaging protocol included axial T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequences for localization, followed by untriggered true-fast imaging with true-FISP cine MRI of the heart. Standard fetal echocardiograms also were obtained.
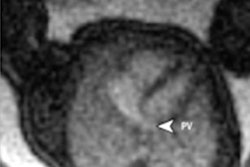
According to the results, the fMRI exams showed long-axis and short-axis views (end diastole and end systole) of the ventricle, ductus venosus, pulmonary artery, ductal arch, and descending aorta. In the patient with diaphragmatic hernia, imaging helped determine that the left ventricular and ascending aorta represented hypoplastic left heart syndrome. The fetus was delivered at 35 weeks and died at 45 minutes of age.
For the second patient, a third echocardiogram continued to show ductal constriction and RV hypertrophy. The fetus was delivered at nearly 30 weeks and the patient continues to do well. "Functional data obtained by MRI aided in the medical decision-making process in this case," the authors stated.
The factors that made fetal cardiac fMRI possible were sedation, a single-shot imaging technique, and the high signal-to-noise ratio achieved with true-FISP, the group concluded. The authors added that by imaging for 49 seconds, and acquiring 320 images, they were able to compensate for "crude temporal resolution, given the fetal heart rate of 133 BPM."
By Shalmali Pal
AuntMinnie.com staff writer
October 7, 2005
Related Reading
MR may be sounder than sonography for catching fetal abnormalities, November 29, 2004
MRI demonstrates fetal thymus, bronchial obstruction, May 12, 2003
Copyright © 2005 AuntMinnie.com