In the parlance of modern youth, the term "phat" is used as an expression of approval, a way to denote that something or someone is attractive or admirable. But the more traditional version of the word also applies to today's youngsters: In 2003-2004, 17.1% of U.S. children and adolescents were overweight or obese, according to a recent study, and this negative trend continues to grow (Journal of the American Medical Association, April 5, 2006, Vol. 295:13, pp. 1549-1555).
When obesity rears its large, ugly head, other diseases follow suit -- type 2 diabetes, hypertension, and sleep apnea, as well as increased morbidity and mortality. This is especially true for U.S. adolescents who live below the poverty line, according to another study that looked at socioeconomic disparities in an obese population (JAMA, May 24-31, 2006, Vol. 295:20, pp. 2385-2393).
Cardiac abnormalities are another issue with overweight children. A group at the Children's Hospital Los Angeles in California studied 109 substantially overweight 8- to 16-year-olds and found that nearly half had multiple risk factors associated with metabolic syndrome. Obese adolescents also suffer from excessive cardiac mass and left ventricular dysfunction (Pediatrics, June 2006, Vol. 117:6, pp. e1111-1118; Journal of the American College of Cardiology, June 6, 2006, Vol. 47:11, pp. 2267-2273).
Fortunately, imaging tests can guide the treatment of obese patients, whether they're used as risk predictors or in postsurgical follow-up. Researchers from the Cincinnati Children's Hospital Medical Center in Ohio successfully used MRI to measure visceral adipose tissue and noninvasively quantify the amount of intra-abdominal fat in pediatric patients.
For this study -- presented in a poster at the 2006 International Society for Magnetic Resonance in Medicine (ISMRM) in Seattle -- Bernard Dardzinski, Ph.D., and colleagues enrolled 42 children with sleep apnea who were referred for abdominal MRI. The mean body mass index (BMI) was 47.2 for the girls and 43.3 for the boys.
"As part of a larger study in childhood obesity, our center has developed MR imaging techniques and methodology to calculate subcutaneous and intra-abdominal adiposity. This study compares previous manual (tissue segmentation) methods with an automated procedure," they wrote.
Axial T1-weighted images of the abdomen were acquired from the lower end of the xiphoid process to the upper end of the iliac crest on a 1.5-tesla system (LX, GE Healthcare, Chalfont St. Giles, U.K) with a body coil. No sedation was used.
Software written in a semiautomated program developed with Interactive Data Language (IDL, RSI, Boulder, CO) and called Cincinnati Children's Hospital Image Processing Software (CCHIPS) was used to segment the fat and read the DICOM-formatted images. The user selected three different slices to determine adipose tissue volumes: superior, inferior, and umbilicus slices.
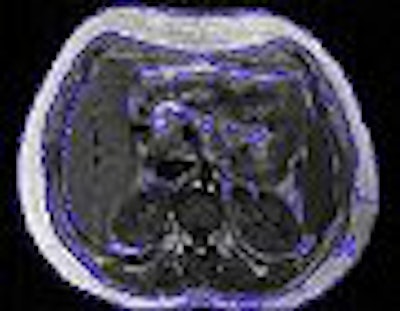
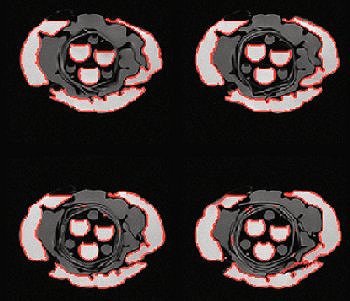
The visceral fat was divided into three adipose tissue volumes: subcutaneous adipose tissue (SAT), intra-abdominal adipose tissue (TAT), and total adipose tissue (TAT). The regions of interest (ROIs) for TAT were obtained using manual and autosegmentation (described in the image below). The mean volumes for all slices were compared using both methods.
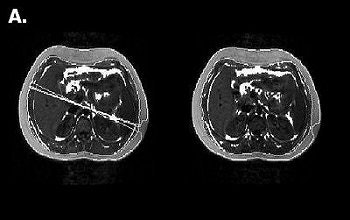 |
| Two slices (nos. 3 and 4) out of 16 and ROI of TAT after segmentation for a 15-year -old boy. Above, automatic (ROI in white). SAT: 3.73 l, IAT: 0.84 l, IAT/SAT: 22.46%. Below, manual (ROI in blue). SAT: 2.23 l, IAT: 0.46 l, IAT/SAT: 20.64%. Images courtesy of Bernard Dardzinski, Ph.D. |
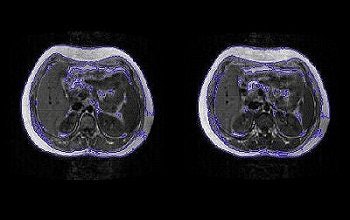 |
The automatic segmentation method was originally laid out in a paper by Dardzinski, Dr. Lane Donnelly, and colleagues. In that phantom study, the group determined the accuracy of using different MR sequences to estimate adipose distribution. They found that conventional T1-weighted spin-echo was not the optimal sequence for measuring visceral adiposity, and recommended a T2-weighted fast Dixon sequence or a T1-weighted 3D spoiled gradient-echo sequence (American Journal of Roentgenology, April 2003, Vol. 180:4, pp. 993-998).
However, Dardzinski told AuntMinnie.com that the segmentation method can be applied "to any imaging sequence when there is good contrast between fat and other tissue. We have better image quality and contrast with T1-weighted fast spin-echo, with multiple 10- second breath-holds. We have used both GRE and SE, and like the better image homogeneity with SE imaging."
 |
| T1-weighted fast Dixon MR images of phantom reveal segmentation process. Signal equal to that of fat is identified. Note structures that contain signal equal to that of fat are outlined in red. Area of each region of interest can be calculated. Volumes can be calculated by adding areas of regions of interest from all axial slices containing area in question. Donnelly LF, O'Brien KJ, Dardzinski BJ, Poe SA, Bean JA, Holland SK, Stephen R. Daniels SR, "Using a Phantom to Compare MR Techniques for Determining the Ratio of Intraabdominal to Subcutaneous Adipose Tissue" (AJR 2003; 180:993-998). |
According to the results of the current study, the mean adipose tissue volumes were significantly correlated between the two methods. The mean values of TAT, SAT, and IAT using autosegmentation were 30% higher than with manual segmentation, but more significantly, the ratio of IAT/SAT was only overestimated by a small amount, the authors stated.
"The IAT/SAT ratio was only 5% higher with the automatic method but the analysis time was reduced 20-fold," they wrote. "This noninvasive technique can be used to monitor weight loss and adipose tissue distribution following bariatric surgery and other treatments for obesity."
This is especially good news as early intervention for adolescent obesity gains acceptance among bariatric specialists. A study presented at the 2006 American Society for Bariatric Surgery meeting in San Francisco found that obese teenagers who had gastric bypass surgery on average lost nearly half their body weight within four years of the procedure. The Brazilian researchers from the Hospital São Camilo in Säo Paolo also stated that the surgery eliminated high blood pressure and type 2 diabetes in the teenagers who had those conditions.
While other modalities such as CT and bone densitometry (DEXA) can be used to measure adipose tissue, they do have drawbacks. "CT has been the gold standard but uses radiation," Dardzinski said. "DEXA can be used, but does not give a clear depiction of the intra-abdominal fat, which is more important than subcutaneous fat. You also only get a projection image from DEXA and cannot quantify volumes."
The reduced scanning and analysis time with the autosegmented MRI method can also help bring down the cost of the scan, he added.
"MRI is expensive but we can do three to four patients per hour because we have reduced the total scan time to less than 10 minutes. Patient compliance is usually not a problem in children over 5 years old. They can remain still (we have video and audio diversion) and can hold their breath for 10 seconds for four times."
Dardzinski said his group will continue to research the use of MRI in this setting. They are currently looking at a cohort of children to determine the correlation between visceral adiposity and other cardiac risks factors, as well as the metabolic syndrome and children with sleep apnea.
By Shalmali Pal
AuntMinnie.com staff writer
July 21, 2006
Related Reading
FDG uptake in obese patients may signal serious cardiac risk, June 7, 2006
Echocardiography more difficult and less accurate in obese patients, May 30, 2006
Enlarged cerebral ventricles predict shortened lifespan, March 8, 2006
Copyright © 2006 AuntMinnie.com