
Posterior ankle impingement (PAI) syndrome is composed of multiple pathologic entities resulting from repetitive or acute forced plantar flexion of the foot. For soccer in particular (or football as it's known in most parts of the world), players' ankles are subjected to chronic forces during jumping, running, and kicking. As a result, chronic ankle pain is a common clinical problem in these athletes.
Recent studies have delved into the diagnoses and treatment of PAI, espousing MRI for the former and ultrasound-guided intervention for the latter. First, Canadian researchers shared their early experience with MR findings in PAI. Then, U.K. investigators looked at the effectiveness of sonographically guided therapy for PAI in soccer players. This same group also voted for MR for pretherapeutic imaging in ankle injuries.
One for all, all for one
In suspected PAI, x-ray may demonstrate the presence of an os trigonum, but that may not be relevant to the problem. In addition, scintigraphy may reveal uptake in the soft tissue and CT can show osseous injury. But MRI is an exam that assesses the full gamut of PAI features, according to Dr. Nathalie Bureau and colleagues from Hôpital Saint-Luc at the Centre Hospitalier de l'Université de Montréal.
"PAI syndrome may manifest as an inflammation of the posterior ankle soft tissues, as an osseous injury, or as a combination of both," they wrote. "MR imaging, with its multiplanar capabilities, exquisite soft-tissue and bone marrow contrast, and large field-of-view availability, is particularly well-suited to investigate foot and ankle disorders" (Radiology, May 2000, Vol. 215:2, pp. 497-503).
The group performed MR exams in seven patients with indeterminate pain in the posterior ankle. One of these patients was a 20-year-old soccer player who had complained of pain in the posterior ankle, which started two weeks after a game.
MRI was done on either a 1- or 1.5-tesla unit (Signa, GE Healthcare, Chalfont St. Giles, U.K). The foot and ankle were in a neutral position with a linear extremity coil, or in plantar flexion with a quadrature extremity coil.
The protocol included transverse, sagittal, and coronal T1-weighted spin-echo imaging; transverse and coronal T2-weighted spin-echo; and T2-weighted fast spin-echo with fat suppression or gradient echo. Bureau and co-author Dr. Étienne Cardinal reviewed the images in consensus.
"We did not grade the severity of abnormalities; rather, we simply classified them as being present or absent," the authors pointed out.
According to the soccer player's results, MR depicted bone marrow edema of the os trigonum, lateral talar tubercle, and subtalar synovitis. No other osseous anomalies and no tibiotalar synovitis or flexor hallicus longus (FHL) tenosynovitis were seen. The PAI diagnosis was established on the basis of MR findings, the group stressed. The patient underwent successful conservative treatment.
 |
 |
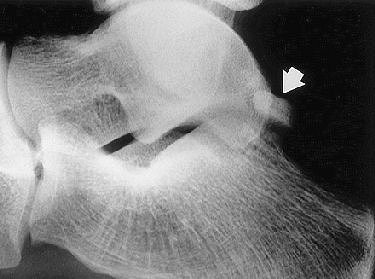
| PAI syndrome in a 20-year-old male soccer player. Above, lateral radiograph of the right ankle demonstrates a well-defined os trigonum (arrow). Middle, sagittal T1-weighted image (366/14) shows area of low signal intensity (arrow) within the os trigonum. Below, sagittal, fast spin-echo inversion-recovery image (4,000/69; inversion time, 130 msec) medial to middle image demonstrates bone marrow high signal intensity (arrows) in the posterior talus, consistent with a bone contusion. |
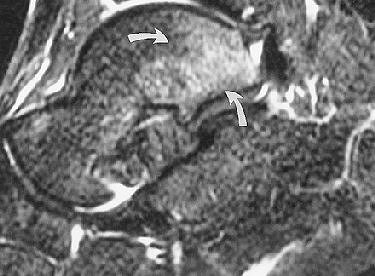 |
| Figure 1abc. Bureau NJ, Cardinal E, Holden R, Aubin B, "Posterior ankle impingement syndrome: MR imaging findings in seven patients." Radiology 2000; 215:497-503. |
In all the patients, "MR imaging findings confirmed the diagnosis of PAI syndrome. MR imaging also had a marked effect on the clinical care by enabling the determination of the exact nature of the osseous and soft-tissue lesions and by excluding other causes of posterior ankle pain," the authors wrote.
Also in all patients, MR depicted low signal intensity of the os trigonum and/or lateral talar tubercle on T1-weighted images, as well as high signal intensity on fat-suppressed T2-weighted imaging. These signs were consistent with bone marrow edema. A major advantage that MR has over x-ray or CT is the ability to depict bone contusions or occult fractures as their presence may influence treatment, they added.
In an e-mail to AuntMinnie.com, Bureau said that, six years later, she still considered MRI to be the best modality for assessing PAI. However, the current protocol at her institution does include a preliminary x-ray, although MRI results are relied upon more heavily for useful information.
Sound treatment
On the MRI exams in the U.K. study, Dr. Philip Robinson from Leeds Teaching Hospitals at St. James University Hospital in Leeds found a preponderance of posterolateral synovitis, thickened posterior talofibular ligaments, and a lack of FHL tenosynovitis
In a study published earlier this year by Robinson, the MR sequence consisted of axial proton density-weighted, sagittal T1-weighted conventional spin-echo imaging; axial, sagittal, and coronal T2-weighted conventional spin-echo fat-suppressed imaging; and gadolinium-enhanced axial and sagittal T1-weighted conventional spin-echo fat-suppressed imaging.
These exams were conducted in a patient population of nine athletes imaged on a 1.5-tesla scanner (Intera, Philips Medical Systems, Andover, MA). On imaging, the posterior ankle was evaluated for synovitis in the posteromedial, posterior, and posterolateral areas.
MR findings included posteromedial capsular thickening, tendon displacement, and posteromedial synovitis in all athletes with posteromedial impingement. Also, all posterolateral athletes had moderate to severe posterolateral synovitis. Bone marrow edema was prevent, but without specific distribution (Skeletal Radiology, February 2006, Vol. 35:2, pp. 88-94).
The focus of Robinson's most recent study, conducted with Dr. Steve Bollen from Bradford Royal Infirmary in Bradford, UK., was sonographically guided injection therapy. "We believe MRI should always be performed before injection to prevent subsequent masking of significant concomitant osteochondral or ligamentous injury," they wrote. "Our study results show a role for sonographically guided steroid and anesthetic injection into the posterolateral capsule abnormality" (American Journal of Roentgenology, July 2006, Vol. 187, pp. W53-W58).
For this retrospective study, they included 10 professional soccer players who had sustained an inversion injury of the ankle in the neutral position. Posterior impingement then developed.
All the players had undergone physical rehabilitation but still developed posterior pain. Both noncontrast and contrast-enhanced MR imaging was done. Ultrasound exams were performed with a 10-15 MHz transducer (Antares, Siemens Medical Solutions, Malvern, PA; ATL 5000, Philips Medical Systems) to evaluate the posterior capsule tissues including a Doppler study of soft-tissue abnormality.
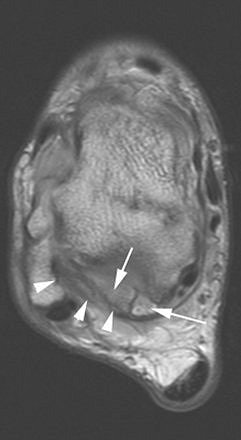
 |
| A 30-year-old male soccer player with clinical posterior impingement. Sagittal T2-weighted fat-suppressed MR image (TR/TE, 3,242/90; echo-train length, 9) shows os trigonum (lower arrow), joint effusion, and nodular posterolateral synovitis (arrowheads) between os trigonum and edematous posterior tibia (upper arrow). |
 |
For the injection therapy, a 20- or 23-gauge needle was inserted directly to the abnormal area of the posterior capsule. Then, 40 mg of triamcinolone acetonide and 3 mL of 0.5% bupivacaine hydrochloride were injected into the abnormal tissues. If an os trigoum was present, the needle was moved on to the ossicle.
According to the results, all patients had posterolateral hypoechoic capsule thickening that was nodular and localized to the lateral aspect of the lateral talar process or os trigonum. All 10 patients tolerated the injection procedure with no immediate complications. They also reported ankle improvement after the bupivacaine shot.
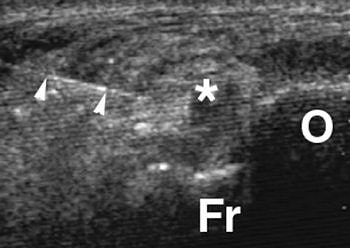 |
| Axial sonography image of os trigonum (O) and adjacent fragment (Fr) obtained during injection shows nodular synovitis (asterisk) with needle (arrowheads) placed during infiltration and injection. Further infiltration was performed around fragments. Robinson P and Bollen SR, "Posterior Ankle Impingement in Professional Soccer Players: Effectiveness of Sonographically Guided Therapy" (AJR 2006; 187:W53-W58). |
The median follow-up time was 26 months for all players. At this juncture, eight out of 10 patients with posterolateral synovitis and no os trigonum had no residual or recurrent symptoms. The remaining two players who did have posterolateral synovitis and os trigonum on imaging experienced a recurrence of symptoms and underwent repeat injection with ultrasound guidance. One player remained pain-free after the second session; the other required endoscopic resection.
With regard to the last two patients, Robinson and Bollen acknowledged that their results were not in line with previous studies on os trigonum, attributing the shorter duration of effective treatment to the complete disruption of the synchondrosis in both patients as well as a higher level of activity.
Ultrasound-guided injection could prove useful for both steroid and anesthetic injections, Robinson concluded. In addition, patients should see a faster recovery time and may be less likely to undergo arthroscopy, he explained (Science Daily News, August 2, 2006).
By Shalmali Pal
AuntMinnie.com staff writer
August 18, 2006
Related Reading
US overcomes x-ray's limits in pediatric ankle fractures, January 23, 2006
Ankle cartilage MRI improved by force, November 28, 2005
Tibial-talar ratio on x-ray reliably shows ankle alignment, May 6, 2005
Soccer players' injury rates tracked in British study, April 22, 2005
Copyright © 2006 AuntMinnie.com




















