Two new studies looked at ways to broaden and improve the role of MRI in uterine cancer, cervical carcinoma, and other cancers in the female pelvis. First, Korean radiologists and radiation oncologists assessed the accuracy of MRI for finding metastatic lymph nodes in cervical cancer patients. In the second study, a group from Germany used a faster MRI sequence on a higher field strength magnet to speed up the imaging process.
MRI in lymph node staging
Clinical staging for cervical cancer is accurate in about 60% of the cases, but the staging guidelines set by the International Federation of Obstetrics and Gynecology (FIGO) do not factor in lymph node metastasis. Nodal metastases can adversely impact survival, said Dr. Hyuck Jae Choi and colleagues from the National Cancer Center in Kyonggi, Korea, and the Seoul National University College of Medicine.
"The presence of a metastatic lymph node radically modifies the prognosis and treatment of cervical cancer patients," they wrote. "CT and MRI have been used to assess para-aortic and pelvic lymph nodes.... However, to our knowledge, no reports define the validity of (MRI) criteria other than size and shape ... in the detection of metastatic pelvic lymph nodes in patients with uterine cervical carcinoma" (American Journal of Roentgenology, November 2006, Vol. 187:5, pp. W538-W543).
For this retrospective study, 55 patients with invasive surgical cancer (FIGO stage IB-IVA) were included. These women were then divided into two groups. The first was made up of patients with stages IB1 (tumor size ≤ 4 cm) and IIA disease. The second group had stages IB2 (tumor size > 4 cm) and IIB disease.
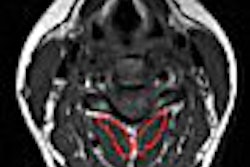
MRI exams were performed on a 1.5-tesla unit (Signa, GE Healthcare, Chalfont St. Giles, U.K.). The imaging protocol included axial T1- and T2-weighted fast spin-echo sequences, a coronal T1-weighted fast spin-echo sequence, and an axial fast spin-echo T1-weighted sequence with 16 seconds of breath-hold to visualize the para-aortic region. All but 10 of the patients underwent gadolinium-enhanced axial and sagittal T1-weighted turbo spin-echo imaging. Two women's imaging specialists interpreted the images.
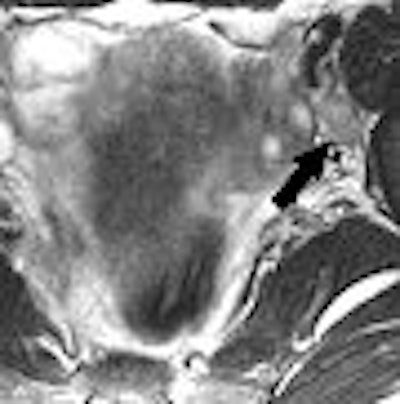
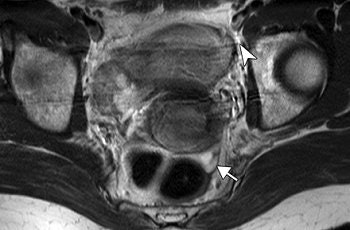
 |
| A 48-year-old woman with true-positive left internal iliac lymph node metastasis in stage IIB uterine cervical cancer. MR axial T2-weighted fast spin-echo image (TR/TE, 5,000/68; echo-train length, 21) shows ovoid lymph node (arrow, 10-mm short-axis diameter) with smooth margin in left internal iliac area. |
According to the results, MRI showed 86 lymph nodes in total and histopathology revealed 17 metastatic lymph nodes in 55 patients. The authors found that the mean short-axis diameter of metastatic lymph nodes was larger than that of nonmetastatic lymph nodes. The sensitivity of this MR criterion was 33.3% and the accuracy was 91.4%.
"The prediction of nodal status was most accurate when a size criterion of greater than 9 mm was applied to the short-axis diameter of the lymph node," the group wrote.
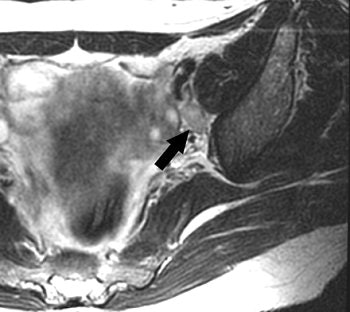
 |
| Same patient as above. Gadolinium-enhanced axial T1-weighted turbo spin-echo sequence image (175/4.2; echo-train length, 3) shows homogeneous enhancement of left internal iliac lymph node (arrow). Histopathology showed one positive node in left internal iliac and obturator area of four nodes sampled. Choi HJ, Kim SH, Seo S, Kang S, Lee S, Kim JY, Kim YH, Lee JS, Chung HH, Lee JH Park SY. "MRI for Pretreatment Lymph Node Staging in Uterine Cervical Cancer" (AJR 2006; 187:W538-W543). |
Other reliable indicators of lymph node status on MR were a lobulated or spiculated border (21% sensitivity and 46.4% positive predictive value). These margins could be caused by a "desmoplastic reaction or tumor infiltration into the perinodal fat." However, heterogeneous enhancement patterns were not as useful for distinguishing metastatic from nonmetastatic lesions, they added.
The group ultimately concluded that despite MRI's low sensitivity, size and margin were useful criteria for predicting lymph node metastasis in cervical cancer patients. But they did caution that size and margins can overlap in metastatic and nonmetastatic lesions.
3-tesla MRI
High field strength MR imaging offers better signal-to-noise ratio (SNR), which can shorten imaging time, but a speedier exam comes at the price of several technical difficulties. Dr. Nuschin Morakkabati-Spitz and colleagues sought to overcome those technical challenges with 3-tesla MRI, sensitivity encoding, and a flip-angle sweep technique.
Morakkabati-Spitz and most of her co-authors are from the University of Bonn in Germany. One contributor, Jürgen Gieseke, is from Philips Medical Systems in Best, Netherlands.
This prospective study was conducted between May and September 2004 in 33 women referred for pelvic MRI. The majority of women had a recent diagnosis, or history of, cervical carcinoma or myoma. Five patients had undergone hysterectomy.
MR studies were done on a 3-tesla unit (Intera, Philips Medical Systems, Andover, MA) with intravenous Buscopan (Boehringer Ingelheim, Ingelheim, Germany) given to reduce peristalsis.
"The turbo spin-echo pulse sequence we aimed to evaluate is based on a single-shot technique and should have markedly shorter imaging time and identical spatial resolution compared with the standard 3.0-T sequence," they explained (Radiology, November 2006, Vol. 241: 2, pp. 538-545).
The sensitivity encoding sequence (SENSE) was used to minimize blurring artifacts. Also, constant level appearance was used for homogeneity correction.
Morakkabati-Spitz and co-author Dr. Marcus von Falkenhausen performed a direct visual comparison between the images obtained with the fast sequence and those taken with the standard sequence. They evaluated signal and image noise.
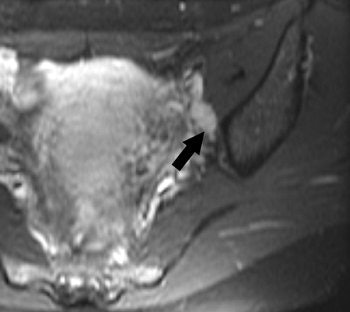
 |
| Transverse T2-weighted MR images in 35-year-old patient with cervical carcinoma obtained with, above, standard sequence (2705/80; imaging time, 4 minutes 3 seconds) and, below, fast sequence (4933/100; imaging time, 39 seconds). Motion artifacts (arrowhead) are absent in image below and moderate in image above; thus, delineation of intact cervical stroma is even better with the fast sequence. Detection of ascites (arrow) is better (in image below). The remaining tissue contrasts and visual SNRs in the two images are comparable. |
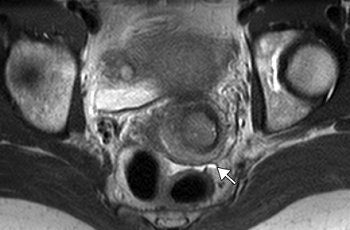 |
| "Female Pelvis: MR Imaging at 3.0 T with Sensitivity Encoding and Flip-Angle Sweep Technique," Morakkabati-Spitz, N, et al. Radiology 2006;241:538-545. |
According to the results, 27 solid tumors were diagnosed in 24 patients and 12 cystic tumors, or liquid-containing disorders, were found in 10. The visual SNR for the fast sequence was comparable to the standard one in all 33 patients. The tissue contrast between solid tumors and muscle also was comparable. With the fast sequence, there was significantly higher contrast between urine and muscle, between ovarian cysts and ovarian stroma, and between cystic tumors or liquids and muscle.
Motion artifacts were significantly reduced with the fast sequence, and the final MRI diagnosis did not differ between the two sequences. On the downside, the tissue contrast of the zonal anatomy could not be analyzed in 33% of the women.
Most importantly, the imaging time for the fast sequence was 39 seconds versus four minutes and three seconds with the standard sequence.
"Fast MR imaging allows increased patient throughput. Furthermore, owing to the reduced imaging time, fast MR sequences allow minimization of motion artifacts, which is especially important in uncooperative patients," the authors wrote.
In addition, the combination of the flip-angle sense technique and SENSE along with the fast sequence allowed for an improvement in diagnostic quality of 3-tesla MRI, they stated. Morakkabati-Spitz told Auntminnie.com that this fast sequence is now used routinely at the Bonn institution, having replaced the traditional 3-tesla sequence.
By Shalmali Pal
AuntMinnie.com staff writer
November 17, 2006
Related Reading
Uterotubal transport abnormal in patients with adenomyosis and endometriosis, September 6, 2006
PET/CT shows strength for staging cervical cancer, May 31, 2006
3D ultrasound brings efficiency gains, May 25, 2006
MRI ready for prime time in cervical cancer diagnosis, November 27, 2005
Copyright © 2006 AuntMinnie.com