
One of the highlight episodes of the popular TV show, "The Brady Bunch" (1969-1973), was "The fender bender." Mom Carol Brady rear-ended the car of Harry Duggan, who then tried to squeeze the Bradys for money by faking a severe case of whiplash. Dad Mike Brady saved the day by throwing his briefcase on the floor in the middle of the courtroom, which startled Duggan into craning his neck around, proving that it was the man's scruples that were really out of whack.
While real-life whiplash cases are not so easily wrapped up, the majority of these injuries resolve themselves, with and without treatment. In some cases the pain and discomfort from whiplash, and whiplash-associated disorders (WAD), can persist for long periods of time. Researchers in Australia and the U.S. relied on MRI to assess why some people experience chronic repercussions from whiplash.
"While the cause for such chronicity is not well understood, it is clear that if symptoms persist for six months following injury, the status of a whiplash patient is unlikely to change significantly," wrote physical therapist James Elliott and colleagues in Spine. "This is the first study ... to show quantifiable MRI changes in the fat content of the cervical extensor musculature, and these changes are present in subjects with no history of neck pain" (Spine, October 15, 2006, Vol. 31:22, pp. E847-E855).
Elliott is an assistant professor in the department of physical therapy at Regis University in Denver. His co-authors are from Regis, as well as from the University of Queensland's School of Medicine and the Centre for Magnetic Resonance, both in Brisbane, Australia.
The patient population for this cross-sectional study consisted of 20 WAD subjects and 32 healthy controls in the U.S. and Australia. At the U.S. facility, images were collected on a 1.5-tesla scanner (Horizon LX, GE Healthcare, Chalfont St. Giles, U.K.) using a conventional spin-echo sequence. In Australia, a 1.5-tesla scanner also was used (Sonata, Siemens Medical Solutions, Malvern, PA). The protocol included T1-weighted axial conventional spin-echo pulse sequences to obtain tissue contrast of fat to muscle.
For the image analysis, regions of interest (ROI) were drawn over each bilateral cervical extensor muscle on the axial T1-weighted images at each vertebral segment (C0-C7). The authors also tested the reliability of MRI in this setting.
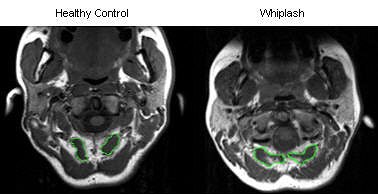 |
| T1-weighted MRI axial scan of C0-C1 (rectus capitis posterior minor outlined in green). |
According to the results, MRI showed a higher level of fat within all extensor muscles in the WAD group. Also in this group, the multifidus muscle showed significantly higher fat content at each level. The largest amounts of intramuscular fat were pinpointed in the rectus capitis posterior minor and major, and the deep cervical multifidi muscles, the authors stated.
"The higher levels of fatty infiltrate in the suboccipital ... and multifidus muscles ... could lead to the contention that there was a greater injury with consequent change in the muscles at these segments. It is possible that those with upper cervical injuries may be more prone to chronicity," the group explained, adding that some of the symptoms associated with WAD -- headache, unsteadiness -- are associated with upper cervical structures.
In addition, the widespread fatty infiltration in WAD patients suggest that the degeneration may result from generalized disuse. The presence of this fatty infiltration could be a consequence of minor nerve injury or irritated and demylineated nerve tissue, brought on by acute inflammatory process, the authors hypothesized.
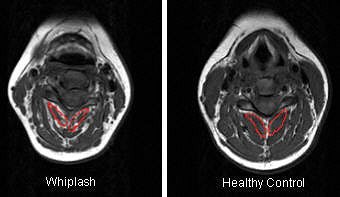 |
| T1-weighted MRI axial slice of the C4 segmental musculature (multifidus muscle outlined in red). |
These results contribute to the expanding cache of literature on MRI and whiplash. Most recently, Dr. Bengt Johansson from Stocksund, Sweden, used functional MRI to diagnose craniocervical joint complex injuries (Pain Research and Management, Autumn 2006, Vol. 11:3, pp. 197-199).
Previously, investigators at the Firda Medical Centre in Sandane, Norway, found a difference in MRI-verified lesions between WAD patients and controls, as well as an association with head position and impact direction at time of accident, indicating that these lesions were caused by the whiplash trauma (Journal of Neurotrauma, November 2005, Vol. 22:11, pp. 1294-1302).
In interviews with AuntMinnie.com, Elliott, who is currently completing his doctorate at the whiplash diagnostic unit at the Centre for Magnetic Resonance at the University of Queensland, shared more details on his group's investigation.
AuntMinnie: How common is persistent WAD?
Data from the U.S. state that just over 16 million reported motor vehicle crashes occur each year. The associated costs related to WAD in the U.S. are staggering, as recent data ("The Economic Impact of Motor Vehicle Crashes 2000") regarding rear-impact crashes report the average total annual cost of whiplash-related injuries to be approximately $2.7 billion ("National Highway Traffic Safety Administration Technical Report," May 2002, pp. 1-94).
Most persons (about 60% to 80%) who suffer a whiplash will recover from their injuries. However, the remaining 20% and up to 40% unfortunately go on to suffer intermittent or chronic pain. Reasons for this transition are emerging and there seems to be a combination of factors, one of which is abnormal or augmented pain processing in the central nervous system.
So persistent WAD is not just phantom pain or brought on by post-traumatic stress?
Whiplash, in the majority of cases, is a real pain (as is evident by the real changes in the muscles identified in our study of chronic whiplash). It is not just a phantom pain, although unresolved post-traumatic stress appears to be one of the predictors for transition to (a chronic condition).
In several published, prospective studies, Dr. Michele Sterling and colleagues at the University of Queensland found that a collection of clinical signs and symptoms -- identified within one month of a whiplash injury -- predicted poor recovery at 12 months and two years for 20% to 25% of the cohort, the type of population used in our recent MRI study (Pain, December 2003, Vol. 106:3, pp. 481-489; Pain, August 2003, Vol. 104:3, pp. 509-517).
The predictive features of a poorer recovery collectively include high initial pain and disability, reduced pain thresholds to cold temperature, reduced range of movement, and psychological distress (Pain, May 2006, Vol. 122:1-2, pp. 102-108; Journal of Psychosomatic Research, April 2006, Vol. 60:4, pp. 387-393).
Sterling's group is currently validating these findings in a larger, multicenter international study.
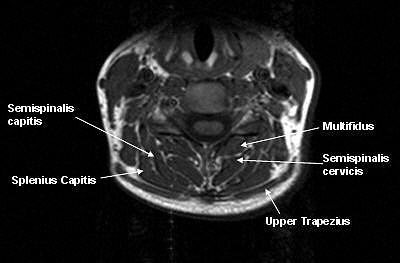 |
| Segmental muscles on T1-weighted MRI axial scan at C6 segmental level in a healthy control. All images courtesy of James Elliott. |
How would information on fatty infiltration gleaned from MRI help with treatment planning? Could it be used to decide if a patient would benefit more from physiotherapy versus muscle relaxants or NSAIDS?
Unfortunately, we cannot answer this question at the moment having just discovered this widespread occurrence of fatty infiltration. However, (our study result) does indicate a deficit in the cervical extensor muscles, and more research is required to determine if specific exercise for these muscles can improve their function, reduce pain and disability, and indeed alter these morphological changes.
We used conventional MRI to quantify these muscular changes (because) we wanted to do a study that was clinically friendly. We wanted (our MRI protocol) to replicate one used in a standard practice, and thus ran a conventional T1-weighted scan of the cervical spine lasting 11 minutes. We also ran standard T2-weighted sagittal scans, but only to set up our axial scans.
Whiplash is not a new condition and has certainly grown in prevalence since the mass production of the automobile. Why have the majority of studies using MRI in WAD been published in the 1990s and early 21st century?
The diagnostic value of MRI in acute whiplash has shown to be poor if the aim has been to identify a salient structural lesion related to symptoms. MRI has often failed to identify an injury whether it is a herniated disk, facet joint, or ligaments.
In response, some have made the argument that because there is no identifiable lesion in whiplash with MRI, the "symptoms" are related to compensation and financial gain.
However, recent Norwegian and Swedish studies have provided strong evidence that WAD patients do present with lesions in the upper part of their necks that are identifiable with specific MRI techniques.
Our measure of fat infiltration is another quantitative measure that can be gained from MRI. At the moment, we are not certain of the mechanisms underlying these changes. It could reflect disuse because of the pain and disability, but there is the possibility of a minor nerve injury.
However, there is much research that needs to be conducted. We do not know how soon following injury these changes occur, but we do know they are established at three months postinjury. We are currently investigating the time frames and establishing relationships to clinical symptoms.
Given that whiplash is a common personal injury claim following a car accident, could MRI be used (or possibly abused) in a legal setting?
It is too early to use the presence of fatty infiltrate (on MRI) in a legal setting, because knowledge is insufficient about what it means and its relationship to pain, disability, and recovery. We do not know if it occurs in all whiplash patients, or just some. We do not know when it occurs or whether there is any change with time. We have made the first observation only. More research needs to be undertaken before it could be considered in a medicolegal context.
What are your plans for future research in this area?
We have another paper coming out on the findings in idiopathic, nontraumatic neck pain. We believe we have the makings of a strong MRI diagnostic test for persistent whiplash, but need to undertake more research.
Our future research plans include a prospective, longitudinal study. We do not know how soon following injury these changes occur and this is to be investigated. We will also research if specific exercise rehabilitation strategies can change the fat infiltration, as well as the pain and disability. Ultimately, these studies will help understand the diagnostic and prognostic utility of these MRI findings.
By Shalmali Pal
AuntMinnie.com staff writer
November 16, 2006
Illustration © Mark Stay.
Related Reading
MR sheds light on both clinical, nonclinical causes of chronic low back pain, September 26, 2006
CT more sensitive than spinal fracture x-ray, but has limits, January 30, 2006
Copyright © 2006 AuntMinnie.com




















