Replacing the invasive biopsy procedure may be a "pie-in-the-sky" goal for the image-based screening exam, but the reality is that the unnecessary biopsy is often unavoidable. However, Japanese radiologists and urologists believe that prostate cancer screening with a combination of MR techniques can accurately detect and localize prostate cancer -- and, yes, possibly avoid needless biopsy.
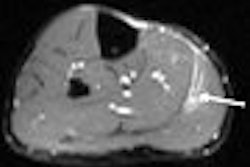
For their study, Dr. Akihiro Tanimoto and colleagues from Keio University in Tokyo included 83 male patients with an elevated prostate-specific antigen (PSA) level of more than 4.0 ng/mL. These patients underwent T2-weighted fast spin-echo (T2W-FSE) MRI, diffusion-weighted imaging (DWI), and dynamic MRI, as well as a transrectal prostate biopsy (gold standard). Imaging was done on a 1.5-tesla scanner (Signa Excite XI, GE Healthcare, Chalfont St. Giles, U.K.). Gadolinium was administered for dynamic MR tests.
Three image interpretation protocols were used:
- Protocol A: data from T2W-FSE
- Protocol B: data from T2W-FSE and DWI
- Protocol C: data from T2W-FSE, DWI, and dynamic MRI
In addition, for DWI, apparent diffusion coefficient (ADC) maps were constructed. ROC analysis (Az) was used to assess the ability of each imaging protocol. For T2W-FSE, low signal intensity in peripheral zone (PZ) and disruption of duct structure were considered malignant.
In DWI, any lesions in the PZ that showed a decrease in ADC were considered malignant. On dynamic MRI, "lesions showing enhancements in the early phase and a washout in the late phase were considered positive," the authors explained (Journal of Magnetic Resonance Imaging, January 2007, Vol. 25:1, pp. 153-159).
According to the results, PSA levels in the 83 patients ranged from 4.3 ng/mL to 332.1 ng/mL. The mean Gleason score of cancerous tissue was 6.9.
The Az values and rates for sensitivity, specificity, and accuracy for each protocol are shown below:
|
For the ROC curves, there were no significant differences between protocol A and B and between protocols A and C, the authors noted. But differences in sensitivity and accuracy could be seen between protocols A and C as well as between A and B for specificity and accuracy.
The authors concluded that in patients with elevated serum PSA levels, protocol C was a valuable tool for detecting prostate cancer and avoiding unnecessary biopsy. Individually, each MR protocol brings something unique to the table. T2W-FSE shows excellent tissue contrast in the prostate and clearly depicts zonal anatomy. DWI coupled with ADC measurements can distinguish benign and malignant lesions. The authors pointed out that their ADC data, which was based on the entire prostate specimen, would be more reliable than ADC data based on biopsy results.
Finally, the usefulness of dynamic MRI in the prostate has been questioned because of overlapping enhancement patterns between normal and cancerous tissue. However, "in our protocol, the scan time of dynamic MRI was 22 seconds and the delay time was 40-180 seconds, which seemed to be a reasonable imaging window to enable peak enhancement of cancer," the group stated.
By Shalmali Pal
AuntMinnie.com staff writer
January 18, 2007
Related Reading
Microflow imaging may boost prostate biopsy yield, December 21, 2006
Dynamic contrast-enhanced magnetic resonance helps spot prostate cancer, November 14, 2006
PET/CT locates tumors within prostate but not outside, October 3, 2006
MR technique, criteria hone in on prostate cancer progression, June 14, 2006
Low-field MR with the right coil tops 3-tesla MR for prostate cancer imaging, December 15, 2005
Copyright © 2007 AuntMinnie.com