When stroke patients undergo standard FLAIR MR imaging, hyperintensity in the cerebral spinal fluid (CSF) can be explained by a handful of causes, such as imaging artifacts, the presence of protein, or the presence of subarachnoid blood.
But gadolinium enhancement in the CSF space caught the attention of Dr. Steven Warach, Ph.D., and Lawrence Latour Ph.D., in the course of their MR studies in acute ischemic stroke. Both researchers are based at the National Institute of Neurological Disorders and Stroke (NINDS) at the National Institutes of Health (NIH) in Bethesda, MD.
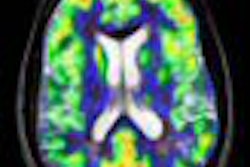
They called this phenomenon hyperintense acute reperfusion marker (HARM) and hypothesized that the presence of HARM was evidence of early blood-brain barrier (BBB) disruption, reperfusion injury, hemorrhagic transformation (HT), and poor clinical outcome. In addition, HARM could serve as a promising new target to broaden the therapeutic window.
"HARM is delayed gadolinium enhancement in CSF space," Warach and Latour wrote in their first paper describing the effect. "The BBB opening indicated by CSF enhancement is distinct from enhancement of the leptomeninges and from the parenchyma enhancement that is observed during the later stage (days to weeks) of ischemia" (Stroke: Journal of the American Heart Association, November 2004, Vol. 35:11, supplement 1, pp. 2659-2661).
In a presentation at the 2007 International Stroke Conference in San Francisco, Warach elaborated on this description of HARM, noting that this particular MR sign has several features: it requires gadolinium enhancement, it's only visible on follow-up FLAIR MRI but not necessarily immediately after stroke onset; it's not seen on T1-weighted imaging; and it's not seen in all stroke patients.
"It really is the presence of the contrast agent in the CSF space," Warach said. He cited the retrospective study he and Latour conducted at the NIH's Suburban Hospital, the results of which were published in Annals of Neurology and Stroke.
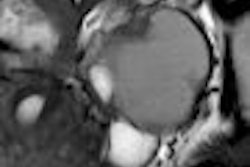
For this research, 213 patients with focal ischemic stroke were first imaged with MR scans within 24 hours of the time of onset, then again at five days and 90 days. Of these patients, 38 had thrombolytic therapy with recombinant tissue plasminogen activator (rtPA), and these subjects had their follow-up at three hours, 24 hours, and 30 days.
Scans were done on a 1.5-tesla scanner using the following sequences: FLAIR diffusion-weighted imaging (DWI), DWI alone, T2*-weighted GRE, spin-echo FLAIR, and perfusion-weighted imaging (PWI).
For data analysis, maps of mean transit time (MTT) were calculate using concentration-time curves obtained from the PWI time series and normalized, the authors explained. There were no instances of CSF space enhancement on FLAIR imaging prior to administration of gadolinium (Gd-DTPA).
"To identify patients having early BBB disruption, we reviewed all FLAIR images sequentially in time. Presence of BBB disruption was identified as positive when the hyperintensity in the CSF in the sulci or ventricles appeared hyperintense in comparison with the previous or subsequent examinations," they wrote (Annals of Neurology, October 2004, Vol. 56:4, pp. 468-477).
Follow-up contrast-enhanced FLAIR images were available in 144 patients. Of these, 33% had evidence of BBB disruption during the first week after onset of ischemia, the group reported. CSF enhancement was seen focally in the sulcal space in the vascular territory of the acute stroke in 21 patients, while 20 patients had CSF enhancement both focally and diffusely within the ventricles. CSF enhancement was seen as late as five days after contrast-enhanced MRI, and the mean time for onset of ischemia to observation of BBB disruption was 12.9 hours.
On perfusion imaging, 85% of the patients had focal ischemia, while 63% had evidence of reperfusion within one week. The authors found that BBB disruption was more common in patients who reperfused than in those who did not, with reperfusion serving as the most significant independent predictor of early BBB disruption.
Finally, among the 121 patients who had acute and GRE imaging follow-up, 18% showed evidence of HT and early BBB disruption was more common in these patients (73%). In addition, patients treated with rtPA were more likely to have HT (31%) and early BBB disruption (55%) than those who did not have rtPA (14% for HT, 25% for BBB disruption).
These results have several implications. First, early BBB disruption is predictive of HT, independent of rtPA and reperfusion. However, the benefits of reperfusion may be hampered by HT and other potential adverse effects. Adjunctive therapy may be required to address BBB disruption and reduce the complications associated with acute thrombolysis, as well as broaden the therapeutic outcome.
"Assuming the Gd-DTPA crossed the BBB within (the) first 1.6 hours after administration, then the estimate of time from onset to evidence of BBB opening is reduced to ... a median of 3.8 hours. This places the timing of the BBB opening close to the treatment time window of acute thrombolytic therapy and makes this event relevant to the development of therapies to prevent HT and improve outcome after thrombolysis or other reperfusion therapy," the authors wrote.
In their second paper in Stroke, Warach and Latour emphasized that reperfusion injury was actually exacerbated by thrombolytic therapy in this same patient population.
"The timing of the disruption is early enough to make it relevant to acute thrombolytic therapy, and the higher proportion of patients exposed to thrombolytic drugs having HARM suggests that early BBB disruption in humans may identify an important target population for adjunctive therapy to reduce the complications," they stated.
By Shalmali Pal
AuntMinnie.com staff writer
June 15, 2007
Related Reading
Advanced MR clarifies nexus between white matter and cerebrovascular disease, February 9, 2007
MRI should be preferred test for suspected acute stroke, January 26, 2007
MRI alters course of thrombolytic treatment for stroke, May 25, 2003
Perfusion CT offers speedy access, but MRI gives the "big" picture, February 19, 2003
Copyright © 2007 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











