Degenerative and herniated disks may lead to potentially disabling disorders and greatly reduce the quality of life of a significant proportion of the population. Degenerative disk disorders are one of the most common presentations to spinal surgeons and one of the most under-researched disorders of the musculoskeletal system (Arthritis Research & Therapy, 2003, Vol. 5:3, pp. 120-130).
For the clinician referring a patient for advanced diagnostic imaging, differentiating normal age-related disk changes from pathological disks can be difficult. MRI plays a vital role in confirming an accurate diagnosis and developing an appropriate treatment plan. This article offers a primer on disk morphology, as well as some guidelines for imaging professionals as to the kind of information clinicians hope to gain from an MR exam.
Discussing disks
While similar to articular cartilage biochemically, the intervertebral disk differs in morphology. It undergoes degenerative changes and aging earlier than any other connective tissue due in part to its avascular nature (Spine, February 15, 2000, Vol. 25:4, pp. 487-492).
The first unequivocal findings of degenerative disk changes may be observed in the 11- to 16-year-old age group; approximately 20% of teenagers may demonstrate mild signs of degenerative disk disease, and degenerative changes of the disk are strongly related to aging, especially in males (Spine, December 1, 2002, Vol. 27:23, pp. 2631-2644).
 |
 |
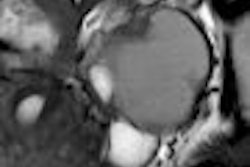
| Above, nonaxial-loaded images. Below, axial-loaded images. Increase in stenosis at L4 level by 2.0 mm and left L4 spinal nerve root with axial loading. All images courtesy of Dr. Gerald Anzalone. |
 |
 |
Ten percent of 50-year-old disks are severely degenerative, while 60% of 70-year-old disks are found to be severely degenerative (Spine, December 1, 2002, Vol. 27:23, pp. 2631-2644).
However, disks in children as young as 2 years old have also been found to show very mild cleft formation with granular changes to the nucleus (Arthritis Research & Therapy, 2003, Vol. 5:3, pp. 120-130).
Disappearing disks
Degenerative disks alter the disk height, load-bearing capacity, and mechanics of the spine. They may alter the integrity of associated spinal ligaments (especially the ligamentum flavum), as well as muscles and connective tissues, and may lead to spinal stenosis. Degenerative disks may be asymptomatic in many cases, but they are strongly associated with lumbar spinal pain in symptomatic cases (Journal of Bone and Joint Surgery: American Volume, September 1990, Vol. 72:8, pp. 1178-1184).
Aging results in fibrosus and the loss of viscosity of the nucleus pulposus, in addition to the loss of integrity of collagen, elastin and proteoglycans. The loss of disk height and fluidity may lead to disk bulging, and areas of stress with associated degenerative vertebral endplate changes correlate to discogenic pain reproduced with discography. Inflammatory responses appear to be associated with symptom-producing disk lesions.
 |
| Above, preaxial loaded. Below, axial-loaded image. Central subligamentous disk herniation and discogenic disease at L5-S1 impressing the thecal sac only after axial loading is applied. L4-L5 bulging, discogenic disease, and a central subligamentous disk herniation impressing on the thecal sac. Bulging and discogenic disease at all other levels. |
 |
Many epidemiological studies have shown that repetitive overload of the spine, poor body mechanics, obesity, and smoking are factors strongly associated with disk-related pain, while other studies suggest that genetic etiologies involving multiple systems and pathways and several different classes of genes are associated with symptomatic degenerative disks (Arthritis Research & Therapy, 2003, Vol. 5:3, pp. 120-130).
Imaging tips
The wide variety of descriptors that clinicians and radiologists use to characterize various disk lesions can be confusing. Several experts have advocated the use of a standardized nomenclature when describing disk pathologies. Disks may be generally categorized as contained (in which the integrity of the outer annulus is preserved) or noncontained.
Contained disks include bulges and herniations. Herniated disks may include focal or broad protrusions or extrusions, depending upon how far the disk has been displaced from the normal boundaries of the vertebral endplate. Noncontained disks may be sequestered, in which a free fragment of disk material (including cartilage, fragmented apophyseal bone, or a fragment annulus) may migrate inferiorly or superiorly with respect to the posterior longitudinal ligament.
 |
| Above and below, axial-load study. L5-S1 anterolisthesis increases from 4 mm to 5 mm with axial loading. L4-L5 retrolisthesis increases from 3 mm to 4 mm with axial loading Mild central spinal canal narrowing. |
 |
Disk displacement relative to the posterior longitudinal ligament may also be subligamentous, extraligamentous, transligamentous, or perforated. The term prolapsed disk may be used synonymously with disk protrusion and may denote inferior migration of extruded disk material (Spine, March 1, 2001, Vol. 26:5. pp. E93-E113).
Axial-loaded imaging of the lumbar spine more accurately demonstrates the conspicuity of disk lesions and other changes related to spinal degeneration. A study by Dr. Shinji Kimura, Ph.D., and Alan Hargens, Ph.D., has shown no difference in the morphology of the lumbar spine between upright imaging and loading the spine in the axial plane at 50% of the patient's body weight. In addition, their research demonstrated that axial-loaded MRI scanning significantly decreased the L4-L5 disk height (Spine, December 1, 2001, Vol. 26:23, pp. 2596-2600).
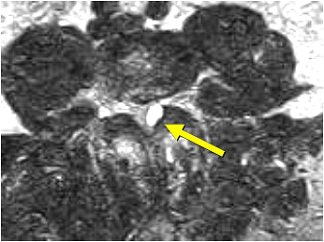
 |
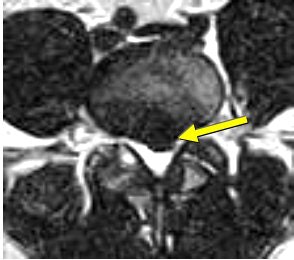
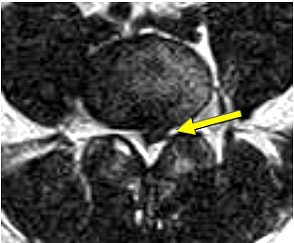
| Above and below, left facet synovial cyst at L4-L5 (1.5 cm superoinferiorly by 1.1 cm anteroposteriorly by 0.8 cm transversely) under axial loading. This synovial cyst caused pronounced compromise of the left lateral recess with severe left lateral recess stenosis, as well as compression and anterior displacement of the left L5 descending nerve root as it exits the thecal sac. The left lateral thecal sac is compressed severely and displaced nearly to the midline. |
 |
In a case report, Dr. Asif Saifuddin and colleagues at Wide Open MRI of North London have shown that axial-loaded lumbar spine imaging increases the sensitivity of the detection of high-intensity zones (Spine, November 1, 2003: Vol. 28:21, pp. E449-E51).
In addition, high-intensity zones may be associated with symptomatic lumbar disk disorders due to annular disruption (Clinical Chiropractic, March 2006, Vol. 9:1, pp. 39-47).
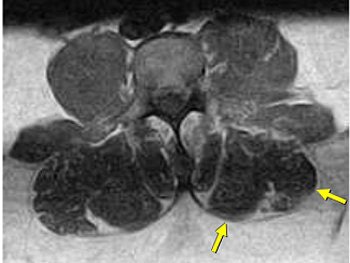 |
| Same patient as above. Left lateral paraspinal muscle asymmetry indicating deconditioning. Axial-loaded images were obtained with the Portal Gravity System. |
Dr. Thomas Gilbert's group from the Center for Diagnostic Imaging (CDI) in Minneapolis has suggested that widening of the fact joint space on a standard MRI is a strong predictor of segmental instability and lumbar spinal stenosis, particularly if the patient is being evaluated for radicular pain or suspected stenosis (CDI Consult, Winter 2005).
They recommend that when widened facet joint spaces are demonstrated in conventional scans in these symptomatic patients, axial-loaded MRI sequences should be performed for dynamic evaluation of the spine, especially in patients 40 years of age or older.
They also reported that the size of a disk herniation on MRI does not determine which patients will respond to conservative management and which patients will ultimately require surgery. They stated that the criteria for the surgical management of a disk herniation are radicular pain, which is unresponsive to six weeks of conservative therapy; uncontrolled pain; major or progressive neurological deficit; and cauda equina syndrome.
Clinicians referring patient for lumbar imaging are generally interested in ruling out the following:
- Neural compromise due to stenosis, arthrosis, osteophytosis, discopathy, or perineural and synovial cysts
- In cases of disk derangement, the specific type of disk abnormality or change in morphology with appropriate standardized terminology
- Segmental instability, anterolisthesis, or retrolisthesis (assessed with axial-loaded or upright imaging)
- Central canal, lateral recess, neural foraminal stenosis (best assessed with axial-loaded or upright imaging)
- Disk derangement, bulging, herniation, or sequestration
- Ligamentous and facet hypertrophy
- Paraspinal asymmetry that might indicate deconditioning
- Space-occupying lesions
- Bone marrow changes
- Pathological spinal changes (fracture, neoplasm, tumor, infiltrative processes, infection)
- Altered signal densities indicating pathological processes
- Postsurgical changes with gadolinium studies
- Regions or structures showing increased uptake with contrast medium
Armed with the appropriate diagnostic imaging information, clinicians can:
- Gain more certainty in treatment decisions
- Increase patient confidence
- Reduce potential liability
- Justify treatments to third-party payers
By Dr. Gerald A. Anzalone, D.C.
AuntMinnie.com contributing writer
June 22, 2007
Dr. Gerald Anzalone is a 1997 graduate of the New York Chiropractic College in Seneca Falls, NY. He is a consultant for Portal Medical of Logan, UT. Anzalone is a member of the Foundation for Chiropractic Education and Research and the American Public Health Association. He practices in Peekskill, NY.
Related Reading
Axial-loaded imaging of lumbar spine heightens diagnostic accuracy, May 29, 2007
Cortical defects on prevertebroplasty MR ups risk of cement leakage, April 3, 2007
Disk transplantation shows promise as treatment for spine disease, March 27, 2003
Copyright © 2007 AuntMinnie.com