Despite steady decreases in mortality rate, prostate cancer remains a significant health concern in the U.S. An estimated 234,460 men were diagnosed with the disease last year. For obese men (those with a body mass index [BMI] of 30 or higher), preliminary research seems to show that, although they may not be necessarily susceptible to a higher incidence of prostate cancer, they are susceptible to more aggressive cancer and higher mortality rates.
According to Alan Kristal, Dr.P.H., associate head of the cancer prevention program at Fred Hutchinson Cancer Research Center in Seattle, obese men have a 30% higher risk of dying of prostate cancer and are 60% more likely to get high-grade disease than thin men.
It's hard to tell whether this connection between obesity and high-grade prostate cancer (Gleason score of 7 or higher) is due to obesity per se or the association of obesity with prostate cancer risk by diabetes, according to a study conducted by Zhihong Gong, Ph.D., and colleagues from the Fred Hutchinson Cancer Research Center (Cancer Epidemiology Biomarkers & Prevention, October 2006, Vol. 15, pp. 1977-1983).
Researchers found that in comparison with men whose BMI was less than 25, obese men had a 29% increased risk of high-grade prostate cancer. Another of Gong's studies found that obesity at time of diagnosis was associated with increased risk of prostate cancer metastasis and mortality (Cancer, March 15, 2007, Vol. 109:6, pp. 1192-1202).
PSA problems
Obese men tend to have lower prostate-specific antigen (PSA) concentrations, and some researchers have suggested that these lower PSA counts could be the link between obesity and high-grade prostate cancer (in that the men may not be getting biopsied until the cancer is at a later stage) and have asked the question of whether the PSA test is as effective for obese men as for those who are not. But the question is controversial, according to Dr. J. Kellogg Parsons, assistant professor of surgery at the University of California at San Diego Medical Center.
"We may be encountering a detection bias," Parsons said. "Some researchers think that with the lower PSA levels in obese men, the red flag doesn't get raised soon enough. But instead of questioning whether PSA testing is a valid way to screen this population, a potential means of dealing with this situation would be to simply reset the standards for PSA testing in obese men in order to eliminate that bias."
And the PSA concentration difference between obese men and their fit counterparts is not dramatic, about 0.22 nanograms, according to Kristal, lead author of a recent study that investigates demographic and lifestyle characteristics with PSA concentration (Cancer, January 15, 2006, Vol. 108:2, pp. 320-328).
"The lower PSA concentration scores in obese men could be because obesity changes steroid hormone concentrations," he said. "But obese people also have greater blood volume, so it could also be a dilution effect. In either case, this difference would have little impact on the interpretation of PSA when used as a screening test."
But the PSA test may not be as specific in prostate cancer detection as needed, and not just for obese men, Kristal said.
"The most important thing for detection is to identify those cancers that, if treated, would have different outcomes," he said. "PSA does a poor job with that. It identifies a lot of cancer, but not necessarily the specific ones that we need to find to save lives."
Imaging prostate cancer
Currently imaging is not in widespread use for prostate cancer detection or staging: the PSA test and physical exam are still the primary means of detecting the disease. A crucial goal for prostate cancer imaging is to classify disease more accurately with a mix of anatomic, functional, and molecular imaging data, according to Dr. Hedvig Hricak, Ph.D., of the department of radiology at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York City.
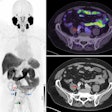
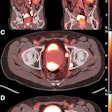
Hricak authored a review in Radiology that summarized the current role of imaging in prostate cancer. Briefly, clinicians use ultrasound to guide biopsies and place brachytherapy seeds and CT to evaluate advanced disease; a combination of CT and PET is sometimes used in treatment follow-up (Radiology, April 2007, Vol. 243:1, pp. 28-53).
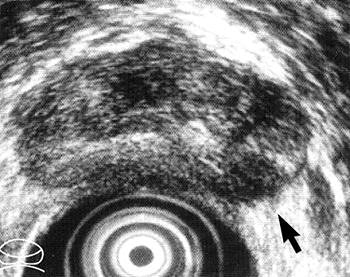 |
| Transverse transrectal ultrasound scan of prostate in 59-year-old man with prostate cancer shows hypoechoic lesion (arrow) in left posterior peripheral zone. Irregular or spiculated margin along the capsule is evidence of ECE of tumor. Focal ECE was confirmed at surgical pathologic examination. Figure 2. Hricak H, Choyke PL, Eberhardt SC, et al. "Imaging Prostate Cancer: A Multidisciplinary Perspective," Radiology 2007;243:28-53. |
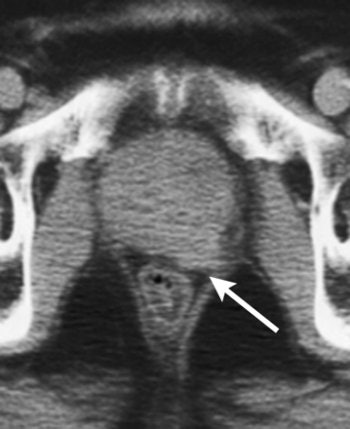 |
| Unenhanced CT scan in 78-year-old man with prostate cancer, Gleason score of 3 + 4 at biopsy, PSA level of 21 ng/mL, and palpable tumor shows enlarged prostate with evidence of gross tumor ECE (arrow) along left posterolateral margin of the gland. Figure 4. Hricak H, Choyke PL, Eberhardt SC, et al. "Imaging Prostate Cancer: A Multidisciplinary Perspective," Radiology 2007;243:28-53. |
MR also looks promising: In a recent study, Japanese radiologists and urologists suggested that prostate cancer screening with a combination of MR techniques could accurately detect and localize prostate cancer, as well as reduce unnecessary biopsies (Journal of Magnetic Resonance Imaging, January 2007, Vol. 25:1, pp. 153-159).
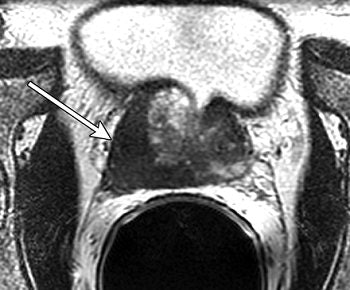 |
| Unenhanced T2-weighted fast spin-echo (5000/96 [effective]) endorectal coil pelvic MR images in 61-year-old man with clinical stage T2a prostate cancer. Transverse image shows a dominant tumor (arrow) at the right base; loss of normal contour and irregular bulging are evidence of extracapsular disease. Figure 8a. Hricak H, Choyke PL, Eberhardt SC, et al. "Imaging Prostate Cancer: A Multidisciplinary Perspective," Radiology 2007;243:28-53. |
They used three different image interpretation protocols (T2-weighted fast spin-echo MRI, diffusion-weighted imaging, and dynamic MRI), and found that the combination of these methods created an accurate and specific picture of disease in men with elevated PSA levels.
In another paper, investigators at the University of California, San Francisco, found that MRI and MR spectroscopy (MRS) were "reasonably accurate" for diagnosing cancer in patients with elevated PSA levels, but that the modalities' limitations made them better suited as an adjunct to biopsy. On the other hand, researchers from Germany stated that MR and MRS offered no diagnostic advantages in prostate cancer over MR alone, especially because MRS had a higher failure rate and a longer postprocessing time in their study (American Journal of Roentgenology, March 2007, Vol. 182:3, pp. 812-816; AJR, September 2006, Vol. 187:3, pp. 724-730).
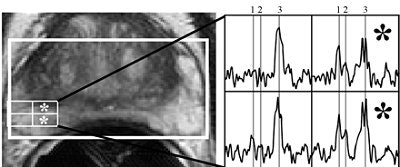 |
| Axial T2-weighted MR image through midgland of prostate in 68-year-old man with prostate-specific antigen value of 6.4 ng/mL and negative findings on one prior biopsy. No focal T2 signal abnormality is visible, but two (asterisks) of four highlighted MR spectroscopic imaging (MRSI) voxels show moderate choline elevation (spectral peaks labeled 1 for choline, 2 for creatine, and 3 for citrate), which is suspicious for malignancy. Cancer was found in right hemigland on subsequent biopsy. Although addition of MRSI to MRI was helpful in diagnosis of prostate cancer in this case, our study showed no overall incremental benefit. Costouros NG, Coakley FV, Westphalen AC, Qayyum A, Yeh BM, Joe BN, and Kurhanewicz J, "Diagnosis of Prostate Cancer in Patients with an Elevated Prostate-Specific Antigen Level: Role of Endorectal MRI and MR Spectroscopic Imaging" (AJR 2007; 188:812-816). |
Meanwhile in molecular imaging, another group found that on delayed or dual-phase FDG-PET, areas of malignancy in the prostate demonstrated stable or increasing contrast medium uptake. More recently, MSKCC investigators tested out PET/CT as a prostate cancer screening tool and found that the results were simply too equivocal (Journal of Nuclear Medicine, February 2006, Vol. 47:2, pp. 262-269; JNM, January 200, Vol. 48:1, supplement 1, pp. 4S-18S).
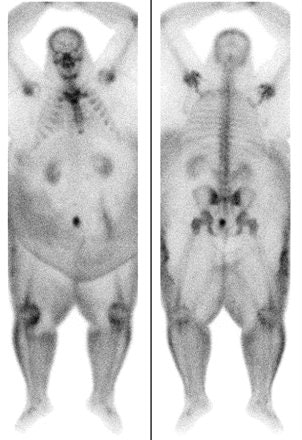 |
| Technetium-99m bone scans in 60-year-old man with suspected osteomyelitis. Photon scatter and soft-tissue attenuation limit image quality. Uppot RN, Sahan DV, Hahn PF, Gervais G and Peter R. Mueller PR, "Impact of Obesity on Medical Imaging and Image-Guided Intervention" (AJR 2007; 188:433-440). |
Could any of these modalities or methods help obese men -- once the PSA level detection bias is corrected? Possibly, Kristal said.
"A different approach to screening for prostate cancer in obese men could work better (than the PSA test) if it revealed something about the biological characteristics of the cancer," he said.
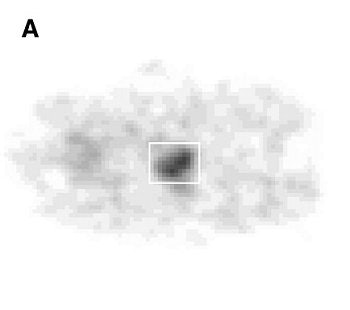 |
| Histopathologic correlation of F-18 fluorocholine PET of prostate. (A) One-hour delayed PET scan of pelvis of subject 14 shows increased F-18 fluorocholine uptake in prostate (enclosed by white box). Kwee SA, Wei H, Sesterhenn I, Yun D, Coel MN, "Localization of Primary Prostate Cancer with Dual-Phase 18F-Fluorocholine PET" (Journal of Nuclear Medicine, Vol. 47, No. 2, 262-269). Reprinted by permission of SNM. |
The logistics of imaging large patients
If it becomes clear that imaging is a good tool in the screening and diagnosis arsenal against prostate cancer, radiologists and technologists will face the physical logistics of comfortably and accurately imaging obese patients. More and more facilities are encountering patients that do not fit on standard imaging tables, and finding that typical imaging parameters cannot penetrate extra layers of tissue. Tissue attenuation becomes a problem in patients who weigh 250 lb or more; larger patients also present a challenge to staff, who have to physically move the patients if the patients can't move themselves.
Imaging vendors are beginning to address this issue by making imaging devices with higher table weights and wider scanner bores to accommodate obese patients. Some MRI scanners can image patients weighing up to 550 lb and have a bigger bore; some CT systems accept up to 680 lb and have a gantry diameter of 90 cm.
But even if the equipment can handle an obese patient, how can technologists get good images? One way to get better images with obese patients is to turn up the power on the equipment, such as high-field MRI or an x-ray unit with high heat capacity because the device may be running for longer periods of time.
In any case, with the increasing trend toward obesity in the U.S., all healthcare workers will find themselves dealing more frequently with larger patients and, in the case of prostate cancer, more aggressive disease. And if imaging is to have a bigger role in screening and diagnosing prostate cancer, not only will imaging equipment have to be made adaptable for obese patients, but the clinical community will have to come to agreement about whether, considering obese men's tendency to high-grade prostate cancer, whether PSA testing alone effectively serves this population.
By Kate Madden Yee
AuntMinnie.com contributing writer
June 7, 2007
Related Reading
High BMI tied to treatment failure in prostate cancer, May 10, 2007
MRI data useful in predicting insignificant prostate cancer, April 24, 2007
Treatments for localized prostate cancer differ in side-effect profile, March 30, 2007
Obesity forces radiology to supersize, enhance x-ray technology, March 1, 2007
ASCO study: Rising PSA, not imaging results, predicts prostate cancer relapse, March 26, 2007
Copyright © 2007 AuntMinnie.com