Introduction
Baker's cyst (also called popliteal cyst) is a type of synovial cyst that represents herniation of fluid through a weakening of the joint capsule. In a Baker's cyst, fluid accumulates around the knee with the gastrocnemio-semimembranosus bursa, resulting in a herniation from the posterior aspect of the knee, through the gap between the medial head of the gastrocnemius and the semimembranosus tendon. The cyst is lined by the synovial membrane and filled with synovial fluid.
Baker's cyst describes cases in which the gastrocnemio-semimembranosus bursa is distended with fluid. In the late 19th century, British surgeon Dr. William Morrant Baker documented eight cases of swelling in the popliteal region, hypothesizing that it was a result of synovial membrane herniation and cyst formation due to osteoarthritis (OA).
Incidence and associations
The incidence of popliteal cysts increases with age, and has been demonstrated arthrographically in 16% of patients in the second decade, 36 % in the third decade, and 54% beyond the fifth decade. Approximately 80% to 90% of popliteal cysts are associated with a meniscal tear, usually medial, although 15% are lateral tears (MRI of the Musculoskeletal System by Thomas H. Berquist, 5th ed., Lippincott Williams & Wilkins, Philadelphia, 2005).
There is also an association with previous meniscectomy, articular cartilage damage (chondromalacia patella and degenerative arthritis), collateral and cruciate ligament injury, loose bodies, rheumatoid arthritis, and other arthritides. Experts have suggested that it is the production of an effusion-producing intra-articular lesion, rather than the specific injury, that is important in the production of popliteal cysts (MRI of the Musculoskeletal System by Thomas H. Berquist, 5th ed., Lippincott Williams & Wilkins, Philadelphia, 2005).
Clinical presentation, complications
In general, patients may present with pain or signs and symptoms suggesting internal derangement of the knee. But they are often asymptomatic and rarely present for the evaluation of a cyst or mass.
In this particular case, a 52-year-old manual farm laborer with osteoarthritis complained of pain in the calf and knee when she bent down to dig in the soil. At time of presentation, she said the pain was incapacitating and that she was unable to work. Her duties included repeated lifting of a 110-lb seed bag, which she positioned on her back by bending her knees and pulling the bag over her shoulder. She also carried firewood on her back in the same way.
For the OA, she had been on nonsteroidal anti-inflammatory drugs (NSAIDs) for two years. Her uric acid levels were normal and she was negative for rheumatoid arthritis (RA) factor. Plain x-rays showed OA of both knees and lumbar spondylosis at L3 through L5.
The patient developed a small effusion in the left knee. She was told to continue her NSAIDs regimen. She was also treated for brucellosis, which was endemic to the region she lived in, but there was no improvement. The effusion grew a little larger and she developed a tender swelling in the popliteal fossa and calf. The pain and swelling worsened as she repeatedly bent and straightened her knee.
Clinically, cysts may dissect into the calf, or rupture and simulate thrombophlebitis. This can lead to hemorrhaging and produce blood products within the cyst.
Pseudothrombophlebitis syndrome describes a deep vein thrombosis secondary to a ruptured popliteal cyst.
Diagnosis and treatment
Patient was referred for a CT arthrogram (as she was unable to pay the hospital fees, her fellow workers pooled sufficient money for her to have the exam and treatment).
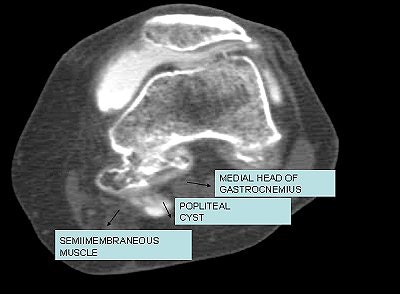 |
| Iodinated contrast-enhanced (8 cc delivered to the knee joint) CT arthrogram (Sytec SRi, GE Healthcare). One-millimeter axial scans (kVp 120; mAs 80) of the joint were performed. There is extravasation of contrast in the synovial cyst between medial gastrocnemius and semimembranosus tendon. Image courtesy of Dr. Shamim Malk. |
At arthrogram, a Baker's cyst and a small medial meniscus tear was diagnosed. The patient underwent excision of the Baker's cyst and medial meniscectomy as the meniscal tear was much larger than perceived on the arthrogram. Her recovery was uneventful and she rested for a full month after the operation.
Follow-up treatment has included physiotherapy for three months (during which the patient shed 4.4 lb). Her knee is now pain-free but it came at the expense of a stiff knee. The surgeon advised that it will take up to a year for knee mobility to return and that she should continue her physiotherapy, which will strengthen her support muscles in months to come. The patient has not had any postsurgical imaging studies done.
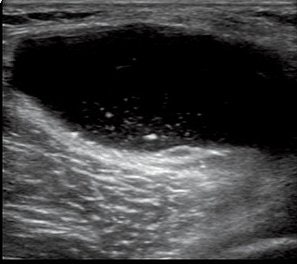 |
| Baker's cyst is one of the risk factors of painful flare in OA of the knee. These patients show a tendency to have an increased rate of Baker's cyst on ultrasonographic findings (Osteoarthritis and Cartilage, June 2006, Vol. 14:6, pp. 540-544). Image courtesy of GE Healthcare. |
Large, painful cysts can be treated with physical therapy, fluid drainage, or corticosteroid medication. If cartilage tear is the reason for overproduction of synovial fluid, surgical repair may be necessary. Baker's cyst related to osteoarthritis may require surgical removal.
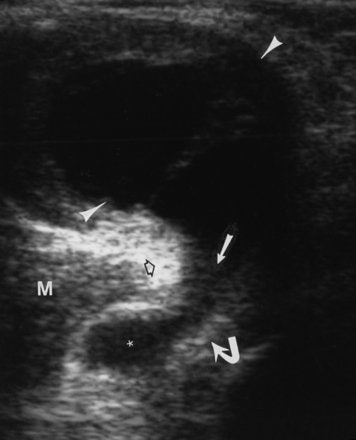 |
| A 60-year-old woman with Baker's cyst. Axial sonogram of posterior knee shows Baker's cyst (arrowheads) with fluid (solid straight arrow) between semimembranosus tendon (curved arrow) and medial gastrocnemius (open arrow). Note subgastrocnemius component (asterisk) of Baker's cyst. Note that top of image is posterior; right side of image is medial. M = medial gastrocnemius muscle. Ward EE, Jacobson JA, Fessell DP, Hayes CW, and van Holsbeeck M, "Sonographic Detection of Baker's Cysts Comparison with MR Imaging" (AJR 2001; 176:373-380). |
Differential diagnosis
Meniscal tear
- Associated with meniscal tear, usually posterior horn of medial meniscus
- Cystic adventitial degeneration of a popliteal artery
- Cystic degeneration of arterial adventitia -- color Doppler ultrasound can be helpful in differentiating popliteal cyst
Popliteal artery aneurysm
- History of sharp trauma
- Color Doppler imaging can confirm the absence of vascular flow within mass, pulsatile, continuous with artery
Ganglion/synovial cyst
- Atypical location compared to popliteal cyst
- Variable location around knee joint
- Tibulofibular joint
- Bursa between lateral head of the gastrocnemius muscle and biceps femoris
- May extend from popliteus tendon sheet/tibulofibular joint
Deep vein thrombosis
- Mimics rupture or leak of popliteal cyst
- Irritating nature of synovial fluid on interstitial soft tissues
- Hyperintense on T2-weighted MRI in soft tissues
- Venous collaterals developing in medial head of gastrocnemius
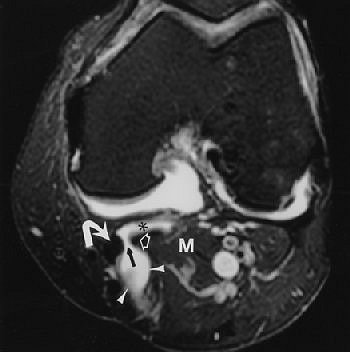 |
| Same patient as above. Axial proton density-weighted MR image with fat saturation reveals Baker's cyst (arrowheads) with fluid (black arrow) between semimembranosus tendon (curved white arrow) and medial gastrocnemius (open arrow). Note subgastrocnemius component (asterisk) of Baker's cyst. M = medial gastrocnemius muscle. Ward EE, Jacobson JA, Fessell DP, Hayes CW, and van Holsbeeck M, "Sonographic Detection of Baker's Cysts Comparison with MR Imaging" (AJR 2001; 176:373-380). |
Semimembranosus tibial collateral ligament bursitis
- Bursal fluid distension
- Hyperintense on T2-weighted MRI
- Inverted U shape
- With or without semimembranosus tendinosis
Both ultrasound and MRI should be considered for confirming a probable benign cyst, such as Baker's cyst, wrote Dr. John Jacobson from the Ann Arbor-based University of Michigan in a review of musculoskeletal imaging. Spanish rheumatologists proposed that ultrasound was particularly useful for assessing periarticular and intra-articular abnormalities involved in the pathophysiology of knee OA (Seminars in Musculoskeletal Radiology, June 2005, Vol. 9:2, pp. 135-149; Osteoarthritis and Cartilage, July 2005, Vol. 13:7, pp. 568-574).
"Musculoskeletal ultrasound allows differentiation of synovial fluid cysts or collections from muscle hematoma and tears, aiding rapid differential diagnosis of a number of causes of musculoskeletal calf pain," stressed another group of rheumatologists from the U.K. Imaging results can guide treatment options such as whether the patient would benefit from injection therapy, they added (Annals of the Rheumatic Diseases, January 2004, Vol. 63:1, pp. 11-14).
By Dr. Shamim Malik
AuntMinnie.com contributing writer
October 18, 2007
Dr. Shamim Malik is a private practice radiologist at the Crater X-Ray Clinic in Nakuru, located in the Rift Valley Province of Kenya.
The opinions expressed in this review are those of the author, and do not necessarily reflect the views of AuntMinnie.com.
Recommend reading
MRI of the Musculoskeletal System by Thomas H. Berquist, 5th ed., Lippincott Williams & Wilkins, Philadelphia, 2005.
Computed Body Tomography with MRI Correlation by Joseph K.T. Lee and Stuart S. Sagel, 4th ed., Lippincott Williams & Wilkins, Philadelphia, 2005.
CT and MRI Imaging of the Whole Body by John R. Haaga, Charles F. Lanzieri, Robert C. Gilkeson, 4th ed., Elsevier Health, St. Louis, 2002.
Diagnostic Imaging: Orthopaedics by David Stoller, Phillip Tirman, Miriam Bredella, AMIRSYS, Salt Lake City, 2003.
Grainger & Allison's Diagnostic Radiology: A Textbook of Medical Imaging by Ronald G. Grainger, David J. Allison, Adrian K. Dixon, 4th ed., Elsevier Health, St. Louis, 2001.
Related Reading
Case study: Ovarian dermoid cyst, June 21, 2007
Part II: Choosing between MR and US in musculoskeletal imaging, September 15, 2006
Part I: Choosing between MR and US in musculoskeletal imaging, September 7, 2006
Osteopath proselytizes for musculoskeletal US, November 11, 2004
Copyright © 2007 AuntMinnie.com