
Two years ago physical therapist James Elliott, Ph.D., and his co-authors conducted a study that connected the chronic pain associated with whiplash and MR signs of fatty infiltrate in the cervical extensor muscles. At the time, Elliot told AuntMinnie.com that his group believed they had the "makings of a strong MRI diagnostic test for persistent whiplash, but (we) need to undertake more research."
That's just what the investigators did, releasing the results of another study in Clinical Radiology. This time, they investigated the presence of fatty infiltrate in patients with nonwhiplash-related neck pain.
In the 2006 MRI study, Elliott and colleagues studied 20 subjects with whiplash-associated disorders and compared them to healthy controls. Based on T1-weighted MR imaging, the authors found a higher level of fat within all extensor muscles in the whiplash group.
In addition, the patient group showed significantly higher fat content at each level of the multifidus muscle, with large amounts seen in the rectus capitis posterior minor and major and the deep cervical multifidi muscles, the authors stated. At the time, Elliott and colleagues hypothesized that the widespread fatty infiltration in whiplash-associated disorders, and subsequent pain and disability, may result from generalized disuse (Spine, October 15, 2006, Vol. 31:22, pp. E847-E855).
"The fatty infiltrate might be a product of either general disuse or minor nerve injury, irritated, and, subsequently, demyelinated nerve tissue resulting from an acute inflammatory process or a combination of these factors," wrote the authors in their latest study. "If general disuse is the cause, then it might be expected that patients with chronic neck pain ... would also ... demonstrate these findings" (Clinical Radiology, January 31, 2008).
Elliott is an assistant professor in the School of Physical Therapy at Regis University in Denver. He is also a postdoctoral research fellow at the Centre for Clinical Excellence in Spinal Pain, Injury and Health and the Centre for Magnetic Resonance (CMR) at the University of Queensland in Brisbane, Australia. His co-authors are from both universities and include Graham Galloway, Ph.D., the group leader of the MR Imaging Group at CMR.
For this research, 23 female patients with persistent, insidious-onset neck pain underwent MR studies on one of two 1.5-tesla scanners (Horizon LX, GE Healthcare, Chalfont St. Giles, U.K; Sonata, Siemens Medical Solutions, Malvern, PA) using a conventional spin-echo sequence. T1- and T2-weighted sequences were done to quantify fatty infiltration to the cervical extensor musculature, the authors explained.
Other information collected on these 23 subjects was hot and cold thermal pain thresholds, pressure pain thresholds, self-reported pain based on the Neck Disability Index (NDI), and the General Health Questionnaire 28 (GHQ-28).
None of these women (mean age 29.2 years) had been involved in a car crash or other trauma that led to a neck injury. Data from these subjects were compared to parallel data from 79 whiplash-associated disorder patients.
According to the MR analysis, "there was a difference in the fat indices of all muscles with (whiplash-associated disorder) participants demonstrating significantly higher amounts of total fatty infiltration when compared with the insidious-onset neck pain participants," the group stated.
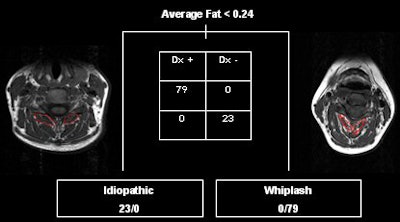 |
| Classification tree illustrating the determination of the condition based on average MRI fat in cervical extensor musculature. Image courtesy of James Elliott, Ph.D. |
Also, those with chronic neck pain had significantly lower NDI scores but pain of longer duration than those with chronic whiplash-associated disorders. The group also found significant differences in hot and cold thermal pain thresholds, with the chronic whiplash patients demonstrating reductions in both. Finally, a significant difference was found in local and remote pressure pain thresholds, again with whiplash patients demonstrating reduced thresholds.
The authors came to several conclusions based on their results. First, that the insidious-onset neck pain group could be distinguished from the whiplash group by the average muscular fat and cold pain thresholds. Second, that the occurrence of cold allodynia and muscle fatty infiltrate in chronic whiplash-associated disorders may suggest common underlying mechanisms such as peripheral nerve injury.
Finally, with regard to their original theory on disuse, the authors stated: "If disuse were the primary or only cause of fatty infiltrate, then it would be expected to be present in those suffering neck pain of a longer duration.... This novel finding may enable a better understanding of ... chronic whiplash."
While disuse may not be the culprit in chronic whiplash-associated disorders, fatty infiltrate could definitely be seen as a hallmark of the disorder, Elliott stated in a recent e-mail interview with AuntMinnie.com.
"We hypothesized that subjects with nontraumatic neck disorders would have less fat content when compared to those with traumatic whiplash. What did surprise us was that the fat index values for the insidious-onset neck pain group mirrored those with no history of neck pain," he said. "These findings help provide more mechanistic support that fatty infiltrate is the result of a possible nerve injury and/or processes related to trauma -- e.g., inflammatory response with subsequent disuse of muscle in the long term."
These results also give MR more weight as a diagnostic tool for evaluating persistent whiplash, Elliott added.
"The accuracy of this (MR-based) system is exceptional -- e.g., the application of a 'cutoff' score for average fat index at less than 0.24 results in a 0% misclassification rate for the condition," he explained.
With regard to treatment, the jury is still out as to how effectively MR results can direct patients with whiplash-associated disorders to the right therapy. But Elliott's group is currently working toward that goal, taking a closer look at the pathophysiological mechanisms of fatty infiltration and whether its presence is prognostic for poor recovery.
"We still need to determine the temporal development of fat, and whether the presence and magnitude of fatty infiltrate will influence clinical decision-making," Elliott said. "Our group currently has two trials ongoing: a longitudinal investigation into the temporal development of fat following whiplash injury, and a trial ongoing that is investigating whether specific therapeutic exercise changes the content of fatty infiltrate in the cervical extensor muscles in patients with chronic whiplash-associated disorders. We will know more later this year."
"We are also working toward more appropriate, multidisciplinary management strategies for the acute and chronic condition," he added.
By Shalmali Pal
AuntMinnie.com staff writer
February 15, 2008
Related Reading
Lapbelt injuries and seatbelt syndrome should trigger search for severe injury, August 29, 2007
Axial-loaded imaging of lumbar spine heightens diagnostic accuracy, May 29, 2007
MR study shows how whiplash can be perpetual pain in the neck, November 16, 2006
Copyright © 2008 AuntMinnie.com




















