
Through the use of functional MRI (fMRI), researchers at the Massachusetts Institute of Technology (MIT) in Cambridge are shedding light on the underlying neural mechanism at the root of macular degeneration.
Authors from MIT's McGovern Institute for Brain Research and the Department of Brain and Cognitive Sciences say that the study shows changes in neural response in people with macular degeneration are probably driven by the lack of input to a population of neurons, rather than a change in visual information processing strategy.
The study appears in the March 4, 2009, issue of the Journal of Neuroscience (Vol. 29:9, pp. 2768-2773).
Macular degeneration is the most common form of adult blindness, whereby some 1.8 million Americans progressively lose vision in the center of their visual field, depriving input to that part of the visual cortex.
Vision loss
Loss of vision begins in the fovea of the retina, the central area of the eye that provides high-acuity vision for reading and other visual tasks. Previous research has noted that the deprived neurons begin responding to visual input from another spot on the retina, which shows evidence of plasticity in the adult cortex.
People with macular degeneration will compensate for the loss of center vision by using an adjacent area of undamaged retina to see objects and function as normally as possible. This so-called preferred retinal locus (PRL) is often below the blind region, prompting adults to adjust their eyes in one direction or another, often upward, to see the object directly in front of them.
"People with macular degeneration lose photo receptors, so cells in the retina in the eye die," explained co-author Daniel Dilks, a postdoctoral fellow in MIT's Kanwisher lab. "By looking up, they are trying to push that blind region out of the way and use the good piece of their eye to view."
The visual cortex has a map of the visual field on the retina, and in macular degeneration, the neurons mapping to the fovea no longer receives input. Several labs, including the Kanwisher lab, previously found that the neurons in the visual cortex that once responded only to input from central vision begin responding to stimuli at the PRL, essentially reorganizing the visual map.
Cortical change
The goal of the recent MIT study was to determine if the chronic, prior use of the PRL causes the cortical change that was seen in the past or if the deprived neurons respond to stimulation at any peripheral location, regardless of prior visual behavior.
The study tested both the PRL and another peripheral location, using fMRI to scan two macular degeneration patients with no central vision and a deprived central visual cortex. The researchers theorized that because patients used the PRL like a new fovea for many years, the deprived cortex might respond preferentially to this location.
However, the researchers discovered that the deprived region responded equally to stimuli at both the preferred and nonpreferred locations. "The reorganization seen in functional MRI literally means that I can see a piece of cortex light up that would never light up [in people with normal vision], because the stimulation in that piece of cortex is not the stimulation that piece of cortex responds to," Dilks said.
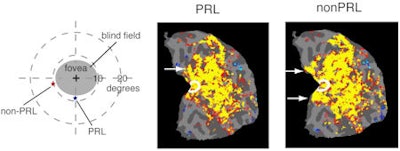 |
| The yellow area inside the white circles in both images shows that the central vision cortex responds to stimuli presented at the preferred retinal locus (PRL) and non-PRL. The bright areas are an indication that reorganization happens in both cases and does not depend on a person using a new part of the retina for many years. Images courtesy of MIT and the Journal of Neuroscience. |
The results suggest that the long-term change in visual behavior is not driving the brain's remapping, but rather the brain changes appear to be a relatively passive response to visual deprivation.
MIT researchers see the findings as an opportunity to learn more about plasticity in the adult cortex and perhaps, eventually, to develop technologies to replace lost light-sensitive cells in the fovea so patients may recover central vision, as the neurons there are still alive and well.
By Wayne Forrest
AuntMinnie.com staff writer
April 8, 2009
Related Reading
MRI distinguishes optic neuropathy due to cat scratch disease, July 5, 2005
Ultrasound brings eye imaging into sharp focus, May 25, 2004
Interventional radiologists may be at risk for posterior subcapsular cataracts, March 30, 2004
Radiotherapy plus thermotherapy provides good local control of uveal melanoma, July 26, 2002
MRI trains an eye on orbital Lyme disease, June 10, 2002
Copyright © 2009 AuntMinnie.com




















