
Physicians at Children's Hospital of Philadelphia are using a unique new method for manipulating 3D cardiac MR images to compare how alternative approaches affect blood flow and expected outcomes. They've found that the technique helps them choose the best course of action prior to an operation.
Pediatric cardiologists and surgeons at the hospital developed a tool for virtual surgery in collaboration with researchers from the Georgia Institute of Technology in Atlanta. Details are featured in the Journal of the American College of Cardiology: Cardiovascular Imaging (August 2009, Vol. 2:8, pp. 1024-1030).
Technology helps determine the best blood flow and the optimum mixture of blood to maximize the heart's energy efficiency, according to Dr. Mark Fogel, an associate professor of cardiology and radiology and director of cardiac MRI at Children's Hospital.
The new tool helped in the case of a 4-year-old girl who was born with only one functional ventricle. Children with this condition suffer from low levels of oxygen in their tissues because the blood mixes in only one functional ventricle before being redistributed to the lungs and the rest of body.
Open-heart surgeries
These children undergo a series of three open-heart surgeries to reshape the circulation in a way that allows oxygen-poor blood to flow from the limbs directly to the lungs without traveling through the heart. Although these vascular modifications can eliminate blood mixing and restore normal oxygenation levels, surgeons and cardiologists must ensure that the lungs will receive proper amounts of blood and nutrients after the surgery so normal development occurs.
The 4-year-old patient in the JACC paper had undergone all three stages of the procedure at Children's Hospital, but she developed severe complications. Her oxygen saturation was as low as 72%, compared with normal levels of at least 95%.
To improve blood flow to both lungs, surgeons needed to operate again and reconfigure the patient's cardiovascular anatomy. Physicians are able to use 3D MRI to model different connections to simulate optimum blood flow characteristics before surgery, noted Dr. Thomas Spray, chief of the cardiothoracic surgery division at Children's Hospital.
Five-part process
The process includes acquiring MR images of the child's heart at different times in the cardiac cycle, modeling the preoperative heart anatomy and blood flow, performing virtual surgeries, using computational fluid dynamics to model the proposed postoperative flow, and measuring the distribution of liver-derived hormonal factors and other clinically relevant parameters as feedback to the surgeon.
In the case of the 4-year-old girl, researchers generated a 3D model of her cardiovascular anatomy and reconstructed the 3D preoperative flow fields to understand the underlying causes of the malformations.
To do so, Jarek Rossignac, Ph.D., a professor in Georgia Tech's School of Interactive Computing, developed Surgem. The interactive geometric model allowed surgeons to use both hands and natural gestures in 3D to manipulate a 3D computer representation of the patient's anatomy. A Surgem user holds a magnetic tracker or robot arm in each hand and uses them to grab, warp, and bend the 3D model on the computer through hand gestures, guided by real-time graphics feedback.
After analyzing the 3D reconstruction of the failing cardiovascular geometry, the team considered three surgical options.
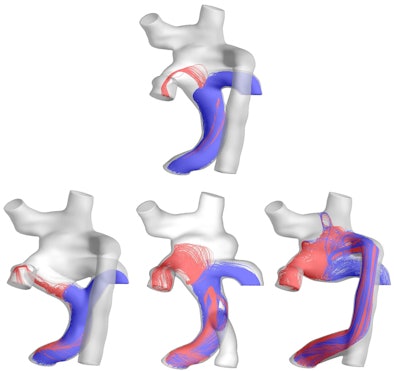 |
| A 3D model of hepatic flow distribution presurgery (top) and postsurgery hepatic flow distribution options (bottom). The surgeon ultimately selected the third option, which exhibited the best performance regarding hepatic factor distribution to the left and right lungs. Image courtesy of Ajit Yoganathan, Ph.D., of the Georgia Institute of Technology and Emory University. |
Surgical solution
The research team performed computational fluid dynamics simulations on all three options to investigate how well blood would flow to the lungs, and the amount of energy required to drive blood through each connection design.
These measures of clinical performance allowed the cardiologists and surgeons to conduct a risk/benefit analysis, which included the difficulty of completing the surgery and potential complications.
Five months after the surgery, the patient showed a "dramatic improvement in her overall clinical condition and oxygen saturation levels, which increased from 72% to 94%," according to the researchers. Currently, the patient's breathing is much easier, and she plays actively like any other healthy child.
This work was funded by a grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health.
By Wayne Forrest
AuntMinnie.com staff writer
August 12, 2009
Related Reading
CMS OKs MRI blood-flow coverage, July 2, 2009
CMS launches national coverage analysis of cardiac MR flow studies, January 22, 2009
Cardiac MR measures predict pulmonary hypertension, April 9, 2007
MR angiography offers greater detail in vascular imaging, March 10, 2006
Copyright © 2009 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











