A large study of children at 23 pediatric hospitals across Canada has yielded a combination of two MRI parameters that predicts the diagnosis of multiple sclerosis (MS) with an accuracy of approximately 90%. The results were published online November 7 in Lancet Neurology.
In addition to demonstrating MRI's prognostic power, the study also indicates that an MS diagnosis can be made shortly after the first attack, rather than waiting months or years until a second attack occurs, according to researchers from the Hospital for Sick Children and the University of Toronto.
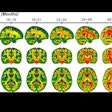
The combination of one or more T1-weighted hypointense lesions and one or more T2-weighted periventricular lesions after an incident demyelinating event is highly predictive of the later diagnosis of MS, the researchers found. Children with both of these characteristics have a 34-fold greater likelihood of being diagnosed with MS than those without either parameter on MRI acquired at the time of acute demyelination.
The results echo aspects of revised 2010 McDonald criteria for MS diagnosis (Annals of Neurology, March 2011, Vol. 69:2, pp 292-302) -- including the importance of periventricular and contrast-enhancing lesions -- but differ in some important ways.
"What's different compared to the 2010 McDonald criteria is that we see MRI evidence of established or chronic disease already at the first attack in the pediatric population, and that's mainly through the T1-hypointense lesions," said lead investigator Leonard Verhey, a PhD candidate. "It will be interesting to determine whether the findings unique to our work will be equally strong predictors of MS diagnosis in adults."
Canadian MS network
The investigators and centers involved in the study are part of the Canadian Pediatric Demyelinating Disease Network, which was launched on September 1, 2004. Data are being gathered prospectively -- including MR studies, clinical data, biological samples, and genetic information -- at the incident event, and then three, six, and 12 months later, and every year thereafter. The MRI analysis involved more than 1,100 scans accrued in 284 children between the network's launch and June 30, 2010.
The 14 parameters examined were distilled from an initial set of 49 that the investigators garnered from the literature, and they represent characteristics that either define MS on MRI or are used in differential diagnosis. A paper is in press that describes the development of the 14-parameter scoring tool.
"These 14 parameters do not require advanced imaging metrics; they are derived from a standard MRI protocol used in the clinical setting," Verhey said. "The application of the parameters also doesn't require specialty training because all parameters are defined in an atlas, and they should be replicable across radiologists and centers due to the high reliability of the parameters."
The analyses
Of 298 children enrolled in the study, 284 were included in the analyses because they had high-quality baseline and subsequent serial scans. Fifty-seven of these children were diagnosed with MS.
Using univariate analyses, the researchers found that seven of the 14 MRI parameters were independently associated with MS and also were associated with interrater reliability coefficients of 0.7 or greater. The presence of one or more T1-hypointensive lesion or of one or more T2-weighted periventricular lesions at baseline were the most strongly associated with MS diagnosis.
This also held true in the multivariate analyses. The presence of both one or more periventricular lesions and one or more T1-hypointensive lesions at baseline had a hazard ratio of 34.27 for diagnosis of MS compared to cases without either of these characteristics (95% confidence interval: 16.69-70.38). The combination of the two features had a sensitivity of 84%, a specificity of 93%, a positive predictive value of 76%, and a negative predictive value of 96%.
The team of investigators also found that the use of its two parameters stands up very well to previously published sets of MRI diagnostic criteria. For example, the 2005 McDonald criteria have a sensitivity of 56%, a specificity of 72%, a positive predictive value of 34%, and a negative predictive value of 87% in the pediatric cohort.
Next steps
Verhey indicated that the team, led by Dr. Brenda Banwell of the Hospital for Sick Children, will continue following the children.
"This research has kindled a momentum from pediatric researchers and clinicians across the country, and we have the information to begin to understand the natural history related to MS on MRI," said Verhey. "The next logical study would be to use this information on natural history of lesion accrual as a segue into defining what an optimal treatment response would be in therapeutic trials of children with MS."


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)





.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)