Monday, November 28 | 3:10 p.m.-3:20 p.m. | SSE01-02 | Arie Crown Theater
The appropriate use of preoperative MRI in selected breast cancer patients can achieve a statistically significant improvement in surgical outcome, according to a new study from researchers at Yale University School of Medicine.The team retrospectively reviewed and identified 158 consecutive patients over a one-year period who underwent initial needle localization and lumpectomy for newly diagnosed breast cancer.
The researchers compared patients who received preoperative MRI with patients who did not in terms of positive margins and re-excisions. They compared factors such as patient age, cancer type, breast density, and surgeon, and determined imaging size and final pathological sizes.
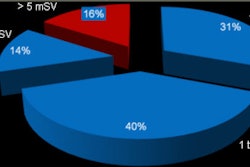
Of the 158 patients in the study, 96 (61%) underwent preoperative MRI. Of those subjects, 13 (13%) had positive margins, while nine (9%) underwent re-excision. Of the 62 patients who did not undergo preoperative MRI, 17 (27%) had positive margins and 11 (17%) underwent re-excision. The difference in positive margins, the authors noted, is statistically significant (p = 0.02).
In addition, positive margins occurred significantly more often in younger women (ages 39 to 49) than in older age groups, and there was a trend for MRI to decrease the positive margin rate among these young women (30%) compared with the older group (60%).
Regarding breast density, positive margins were found in 30% of the fatty breast cases, 11% in scattered cases, 26% in heterogeneous cases, and 20% in extremely dense breasts. The researchers also found that MRI reduced the percentage of patients with positive margins most significantly for heterogeneous breasts.
"MRI provides the best information about the extent of disease, particularly in dense breast tissue where mammography may only show the tip of the iceberg," said presenter Dr. Liane Philpotts, professor of diagnostic radiology and chief of breast imaging. "This information can provide the surgeon with a road map to facilitate removing all or most of the tumor."
Philpotts plans to continue the research by collecting more data and looking closely at the accuracy of MRI for extent of disease in various tumors.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











